JAHA:HIV感染者社区获得性肺炎与心血管事件风险
2020-11-23 MedSci原创 MedSci原创
调整已知的CVD危险因素和CAP严重程度后,PLWH和未感染HIV的患者在CAP住院期间或之后发生CVD事件的风险相似。然而,在多变量校正模型中,HIV感染与CAP住院后30天死亡率增加相关。
未感染HIV的患者因社区获得性肺炎(CAP)住院治疗会增加心血管疾病(CVD)事件的风险。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估CAP住院后,HIV感染者(PLWH)是否比未感染HIV的个体具有更高的CVD或死亡风险。

研究人员分析了美国退伍军人老龄化队列研究2003年4月至2014年12月期间的数据 ,并使用Cox回归分析确定从入院之日起至出院后30天(30天死亡率)期间HIV感染状况是否与CVD事件和死亡率相关,并调整了已知的CVD危险因素。
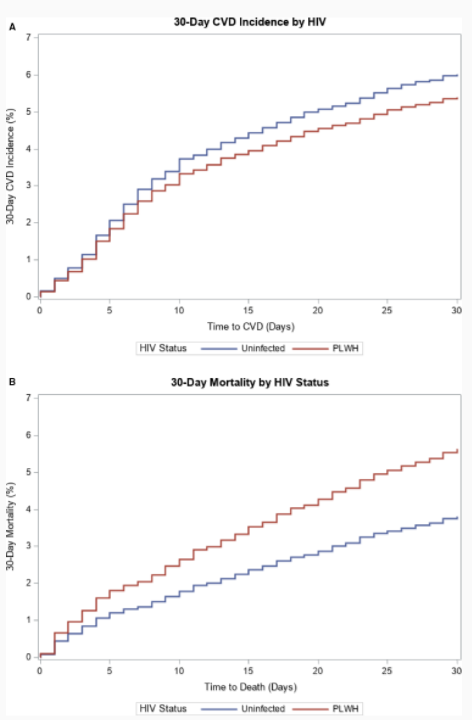
研究人员纳入了4384例患者(67%[n=2951]PLWH)。与未感染HIV的CAP患者相比,因CAP住院的PLWH较年轻,CAP严重程度较低且CVD危险因素较少。在多变量校正分析中,与未感染HIV相比,PLWH个体的CVD风险相似(风险比[HR]为0.89;95%CI为0.70-1.12),但HIV感染与更高的死亡风险相关(HR为1.49;95%CI为1.16-1.90)。在按HIV状况分层的模型中,CAP严重程度与PLWH和未感染HIV的患者的CVD和30天死亡率显著相关。
由此可见,调整已知的CVD危险因素和CAP严重程度后,PLWH和未感染HIV的患者在CAP住院期间或之后发生CVD事件的风险相似。然而,在多变量校正模型中,HIV感染与CAP住院后30天死亡率增加相关。
原始出处:
Jerry S. Zifodya.et al.Community‐Acquired Pneumonia and Risk of Cardiovascular Events in People Living With HIV.J AM HEART ASSOC.2020.https://www.ahajournals.org/doi/10.1161/JAHA.120.017645
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管事件#
36
#获得性#
36
学习了!受益匪浅
0
久违了,学习,学习!
97
受益匪浅,学习,学习。
103
#AHA#
28
#心血管事件风险#
43
#HIV感染者#
38
#社区#
35
HIV感染与更高的死亡风险相关
78