J Oncol:首次报道!LOC105371267变异对中国北方汉族女性乳腺癌易感性的影响
2021-09-11 MedSci原创 MedSci原创
本研究首次揭示了LOC105371267对中国北方汉族女性BC易感性的影响, LOC105371267变异可能是 BC 风险的遗传标记, 或能用于BC 的诊断和预测。
乳腺癌(BC)是女性过早死亡的重要成因,也是最常见的癌症之一。在国外,每年诊断出170万新发病例,120万人死于这种疾病在国内,癌症的健康负担正在不可避免地增加。乳腺癌分为不同的亚型,其独特的生物学、生存结果和相关风险因素不同。
LOC105371267,也称为PR-lncRNA1,是p53调节的长非编码RNA(lncRNA),在乳腺癌的发病机制中起着至关重要的作用。本研究旨在观察LOC105371267多态性和BC风险在中国北方汉族女性的潜在关联。

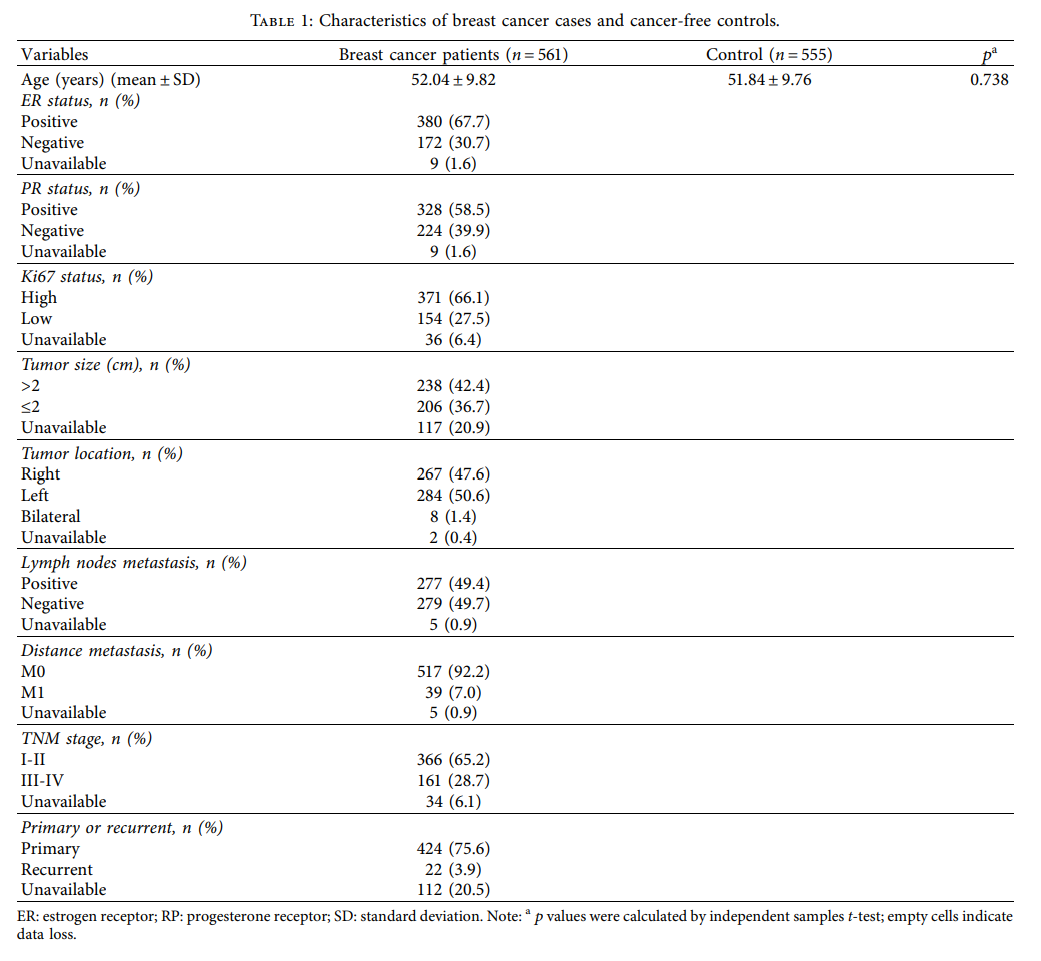
本研究共招募了1116名女性参与者(561名BC患者和555名对照组患者)。在年龄方面,BC病例与对照组之间没有显著差异(p <0.05)。在 561 个 BC 病例中, 380例(67.7%)为ER阳性,328例(58.5%)为PR阳性,371例(66.1%)为Ki-67高表达,238例(42.4%)为肿瘤大小> 2厘米,267例(47.6%)淋巴结转移阳性,517例(92.2%)病例M0转移,366例(65.2%)病例处于I-II TNM阶段,424例(75.6%)为原发病例。
据研究标准筛选了 5 个 LOC105371267(rs6499221、rs3931698、rs8044565、rs3852740 和 rs111577197)的 SNP进行基因型测试。患者与健康对照组(p > 0.05)在等位基因频率上没有显著差异,这意味着这些SNP在等位基因模型中不易受到BC的影响。
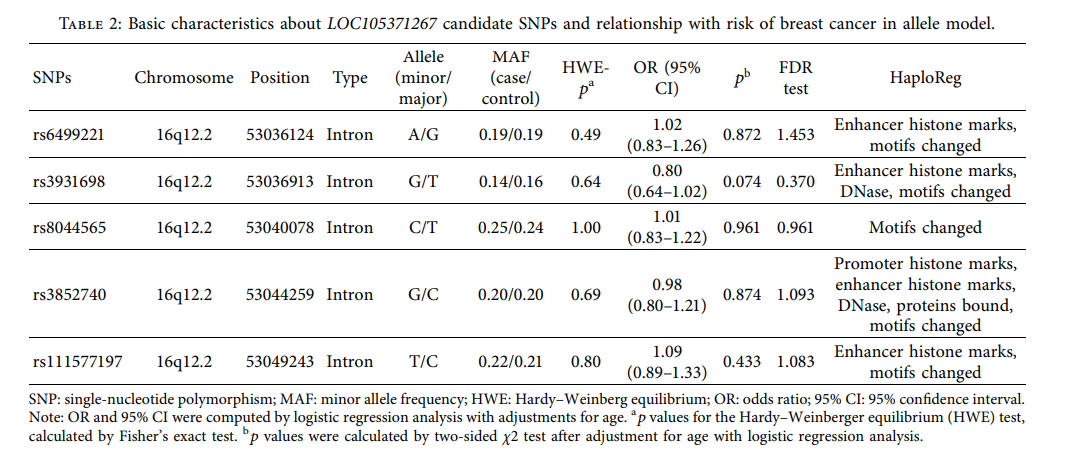
根据年龄调整评估LOC105371267 SNPs与BC风险之间的关系。可见 rs3931698 (GG vs. TT) 的同源性 BC 风险降低了 0.3 倍 (OR = 0.30, 95% CI: 0.11+0.82, p=0.018) 。而在隐性模型(OR = 0.30,95% CI: 0.11+0.84,p =0.021)中,rs3931698的风险降低了 0.3 倍。BC 风险与剩余 SNP(rs64992221、rs8044565、rs3852740 和 rs111577197)之间没有显著的统计差异。

中国乳腺癌诊断的平均年龄在45-55岁,结合本研究所登记的研究对象的平均年龄进行了分层分析。图2可见rs3931698 在同源基因型表现出与年龄在 <52 岁的患者BC 风险降低显著相关(GG vs. TT, OR = 0.26, 95% CI: 0.71+0.97, p=0.045。rs6499221 的异质基因型与年龄为 <52 岁BC 风险增加有关(AG vs. GG, OR = 1.48, 95% CI: 1.01+2.09,p =0.046)。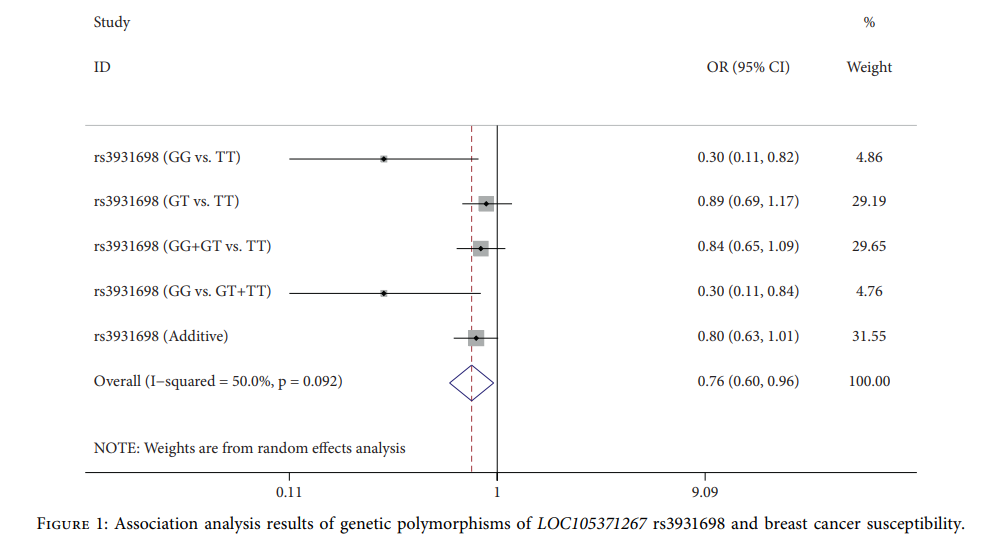
临床特征上, rs3931698 存在增加 PR 阳性 BC 的可能性(GT vs. TT: OR = 1.52) , 95% CI: 1.01+2.29, p=0.043), rs6499221 存在增加 ER 阳性BC 的可能性 (OR = 1.43, 95% CI: 1.02+2.02, p=0.041)。然而,rs3582740 与 ER 阳性 BC的概率降低有关(OR = 0.73,95% CI: 0.53=0.99,p =0.043)。根据 TNM 阶段(III-IV/I-II)进一步评估LOC105371267 SNP 对 BC 严重性的影响。与I-II期(OR = 1.58) 相比,rs3931698的异质基因型在临床 III-IV 阶段的患者中所占比例高。(95% CI: 1.04+2.40, p=0.033), 这表明 rs3931698 对TNM 阶段的不良影响。
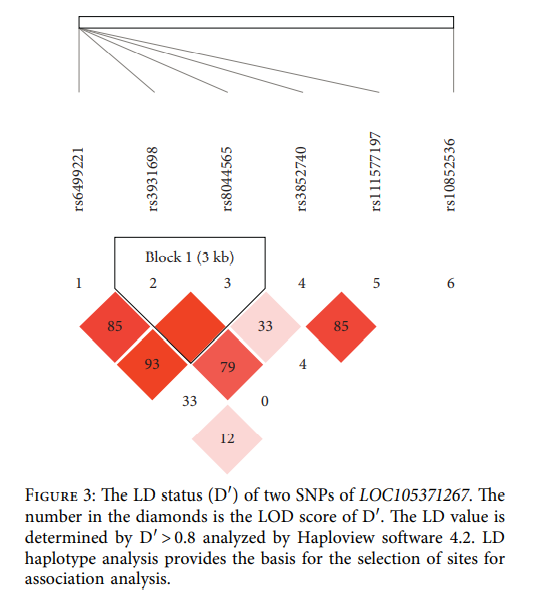
在LOC105371267多态性的单倍型分析中,发现只有两个 SNP, rs3931698 和 rs8044565形成三个单倍型 (TC, GT 和 TT) ,均未与BC的发病率有关(p >0.05)。
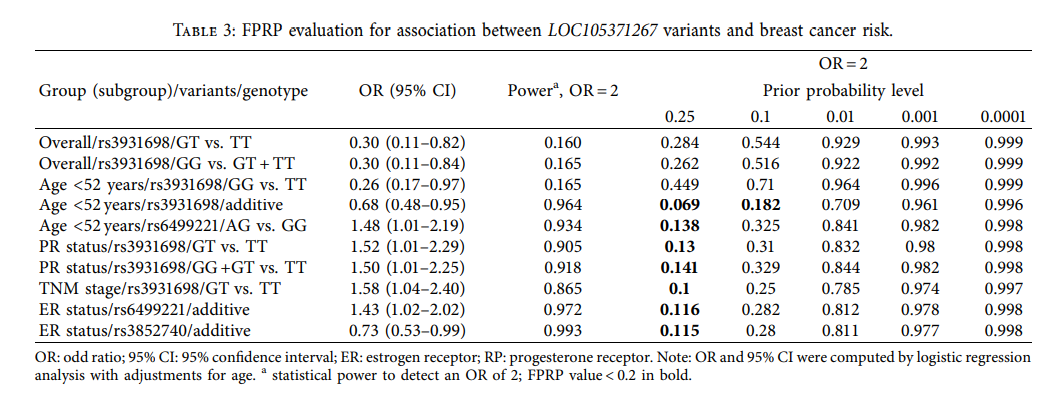
据本研究中的FPRP分析结果显示,当OR值为2时,rs3931698亚组(患者年龄<52岁)的BC风险有显著关联,其FPRP水平在0.1的概率水平下<0.2:此外,其他阳性结果仍具有显著关联。
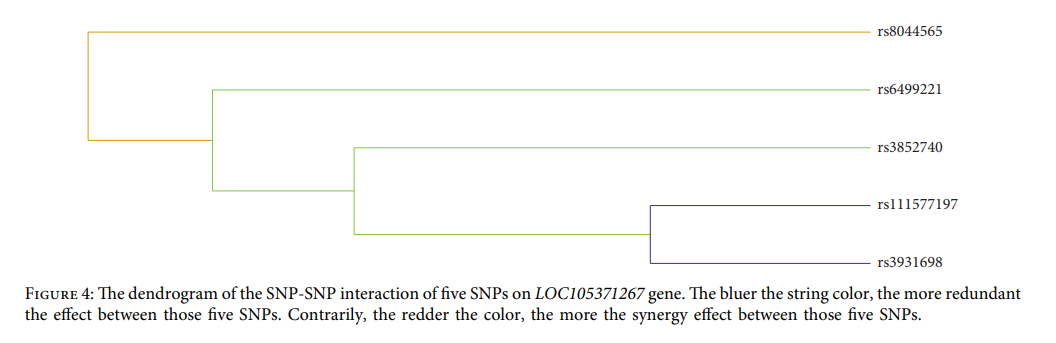
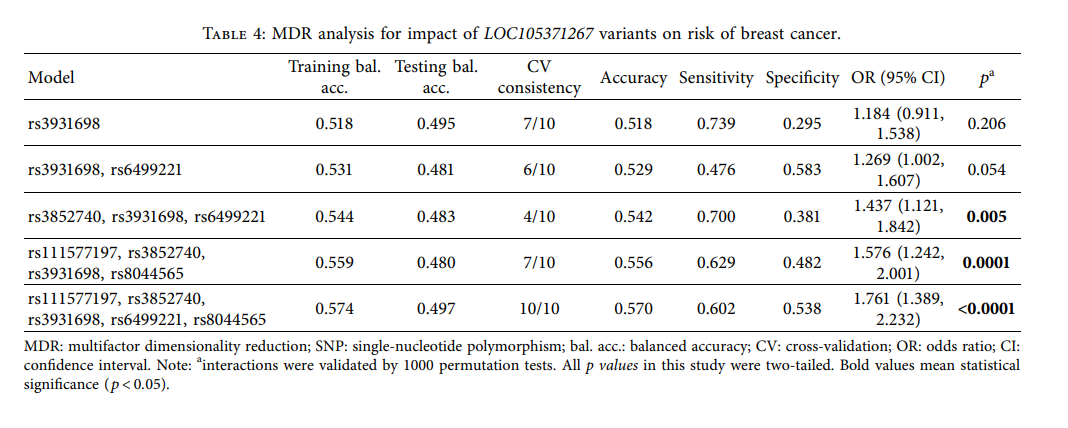
最后,本研究进行了 MDR 分析,以更好地评估LOC105371267变种对 BC 风险的影响。最佳基因型组合是 rs111577197-TT、rs3852740-CC、rs3931698-GT、rs6499221-AG、rs8044565-TC。最佳模型对BC预测风险的影响是显著的(p <0.0001)。字符串颜色越蓝,这五个 SNP 中的冗余效应越大;颜色越红,这五个 SNP 之间的协同效应就越大。
 在这项研究中, LOC105371267 SNPs rs3931698 和 rs6499221 分别与<52 岁的患者 BC 风险降低和增加有关。此外还发现LOC105371267 SNPs(rs3931698、rs6499221 和 rs3852740)或与 BC 的 ER 状态、PR状态和 TNM 阶段相关联。
在这项研究中, LOC105371267 SNPs rs3931698 和 rs6499221 分别与<52 岁的患者 BC 风险降低和增加有关。此外还发现LOC105371267 SNPs(rs3931698、rs6499221 和 rs3852740)或与 BC 的 ER 状态、PR状态和 TNM 阶段相关联。
总之,本研究首次揭示了LOC105371267位点rs3931698、rs6499221和rs3852740多态性对中国北方汉族女性BC易感性的影响, 揭示LOC105371267变异可能是 BC 风险的遗传标记, 这有利于 BC 的诊断和预测。
原始出处:
Impacts of LOC105371267 Variants on Breast Cancer Susceptibility in Northern Chinese Han Females: A Population-Based Case-Control Study. J Oncol. 2021 Aug 28;2021:4990695. doi: 10.1155/2021/4990695. eCollection 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
40
#变异#
31
#易感性#
0
学习了
67
谢谢梅斯分享这么多精彩信息
55
谢谢梅斯分享这么多精彩信息
61