Eur Heart J:HIV感染者的胸腹主动脉瘤发生率升高了4倍!
2021-07-13 MedSci原创 MedSci原创
与未感染的对照组相比,HIV感染者患主动脉瘤的几率高出四倍,而且HIV状态与主动脉瘤独立相关
联合抗逆转录病毒疗法的引入极大地改善了HIV感染者(PLWH)的预后,但HIV感染者的长期存活率仍然低于未感染者,部分原因是HIV感染者的心血管疾病 (CVD) 的发病率增加。据报道,与普通人群相比,HIV感染者发生动脉粥样硬化性CVD的可能性是其两倍。
但是,HIV感染者主动脉瘤的患病率仍未明确。Julie等人调查了HIV状态是否与主动脉瘤独立相关,还评估了与HIV感染者主动脉瘤相关的风险因素。
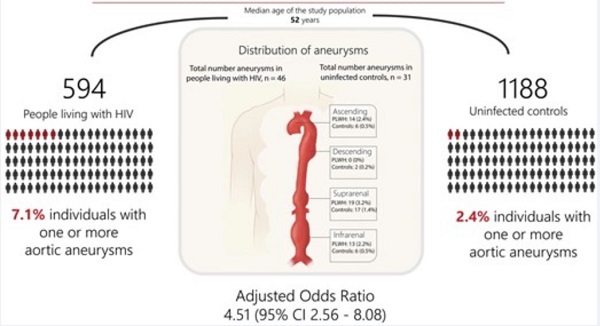
在HIV感染研究中招募了594位40岁及以上的HIV感染者,并从普通人群研究中招募了1188位年龄和性别相匹配的非感染对照。根据欧洲心脏病学会指南定义主动脉瘤:即主动脉扩张≥50%或肾下主动脉直径≥30 mm。
两组受试者的主动脉瘤风险比
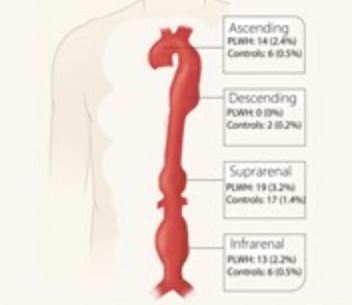
HIV感染者和非感染对照的中位年龄分别是52岁(47-60)和52(48-61),男性分别占88%和90%。在42位(7.1%)HIV感染者中发现了46例主动脉瘤,在29位(2.4%)非感染者中发现了31例主动脉瘤(p<0.001)。HIV感染者的升主动脉瘤和肾下主动脉瘤的患病率明显较非感染者高。在校正模型中,HIV感染与主动脉瘤独立相关(校正优势比 4.51, 95%CI 2.56-8.08;p<0.001)。在HIV感染者中,肥胖和乙肝病毒共感染也与主动脉瘤相关。
总结示意图
综上所述,与未感染的对照组相比,HIV感染者患主动脉瘤的几率高出四倍,而且HIV状态与主动脉瘤独立相关。在HIV感染者中,年龄、肥胖和合并乙型肝炎感染均与主动脉瘤的发生率较高相关。该研究结果表明,增加对HIV感染者主动脉瘤的关注可能是有益的。
原始出处:
Hogh Julie,Pham Michael Huy Cuong,Knudsen Andreas Dehlbok et al. HIV infection is associated with thoracic and abdominal aortic aneurysms: a prospective matched cohort study.[J] .Eur Heart J, 2021, https://doi.org/10.1093/eurheartj/ehab348
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#发生率#
37
学习
0
#HIV感染者#
42
#ART#
44
#主动脉#
41
#主动脉瘤#
32
#HEART#
31
学习了
80
好
69