JOP:比较经喉罩与气管插管给药治疗早产儿的疗效
2023-05-21 小文子 MedSci原创 发表于海南省
经LMA给予表面活性剂治疗不劣于ETT给药,它减少了早期治疗失败,可能是通过避免给药前、喉镜检查和插管的不良反应。
早期表面活性剂治疗对呼吸窘迫综合征(RDS)婴儿有益,并可显著降低不良的肺部后果和死亡率。THE JOURNAL OF PEDIATRICS杂志发表了一项研究,评价经喉罩(LMA)和气管插管(ETT)给药在避免呼吸窘迫综合征(RDS)早产儿机械通气方面可能的非劣效性。
这项随机对照研究纳入妊娠27~36周出生的婴儿,出生体重>800g,诊断为RDS,需要无创呼吸支持,吸氧分数0.30~0.60,持续2h以上,以维持出生48h内血氧饱和度>88%。
婴儿被随机分配通过LMA或ETT接受表面活性剂治疗,ETT组婴儿在插管前接受0.01mg/kg阿托品和2mg/kg瑞芬太尼的术前用药,LMA组婴儿在插入1号LMA Unique(北美LMA)之前接受了阿托品的术前用药。主要结局是表面活性剂治疗失败,需要机械通气,即超过2剂表面活性剂治疗,持续需要FiO2 >0.60以维持目标氧饱和度,或第1次给药后8小时内再次给药。
结果纳入93例患者,随机分配51例LMA组和42例ETT组。两组的基线特征相似,出生体重810~3560g之间。
对主要结局(即表面活性剂治疗失败)的意向治疗分析显示,LMA组的失败率为20%,而ETT组为29%,RR=0.69(95%CI,0.33-1.43;P=0.314)。通过意向治疗进一步检查了失败时间,研究发现LMA组只有1名婴儿(2%)在表面活性剂给药1小时内需要机械通气,而ETT组有5名婴儿(12%)经历了早期治疗失败,具有统计学意义(P=0.044)。
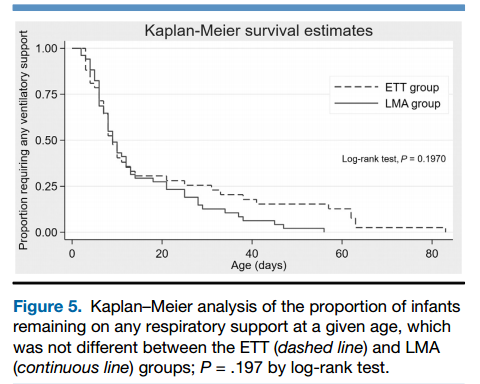
LMA表面活性剂治疗不劣于ETT给药;失败风险差异为9.0%(CI,–∞~5.7%)。各组在减少吸氧量、表面活性剂剂量、停止呼吸支持时间、不良事件发生率以及包括肺气肿和支气管肺发育不良(BPD)诊断在内的结局方面的疗效没有差异。
结果表明,经LMA给予表面活性剂治疗不劣于ETT给药,它减少了早期治疗失败,可能是通过避免给药前、喉镜检查和插管的不良反应。这些特性使LMA成为表面活性剂给药的理想导管。
原文出处:
Jacqueline A. Gallup, Sussan Mbi Ndakor, et al, Randomized Trial of Surfactant Therapy via Laryngeal Mask Airway Versus Brief Tracheal Intubation in Neonates Born Preterm, THE JOURNAL OF PEDIATRICS, 2023, https://doi.org/10.1016/j.jpeds.2022.10.009.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














打卡
53
谢谢分享
43
谢谢分享
48
学习新知识
45
好文章,谢谢分享。
48