Front Oncol:术前放疗(RT)和治疗前CEA水平跟局部晚期直肠癌(LARC)患者预后的关系
2021-10-12 yd2015 MedSci原创
研究表明,治疗前CEA水平被认为是一个潜在的标志物,用于筛查从术前放疗获得长期生存的LARC患者。
术前放疗,无论是长疗程放疗(LCRT)还是短疗程放疗(SCRT),都是治疗局部进展期直肠癌(LARC)的标准新辅助治疗策略。然而,无论是LCRT还是SCRT,术前放疗的长期生存获益仍存在争议。癌胚抗原(CEA)是大肠癌的常规筛查和诊断指标,是广泛应用于大肠癌术后复发的监测标志物。然而,目前还没有关于CEA用于指导术前放疗远期临床预后管理的报道。近期,福建医科大学附属肿瘤医院团队利用SEER数据库,评估局部晚期直肠癌(LARC)术前放疗的长期生存获益情况,并确定术前放疗患者的治疗前CEA水平与预后的关系。相关结果发表在Frontiers in Oncology杂志上。
研究搜集SEER数据库2011年-2015年期间诊断的LARC患者相关资料,根据纳入标准分为手术治疗组(S)和术前放疗续贯手术治疗组((RT+S)。主要结果是癌症特异性生存率(CSS)和癌症特异性死亡率(CSM)。CSS采用Kaplan-Meier分析评估,CSM采用竞争风险模型评估。根据治疗前CEA水平分层进行亚组分析。
共有2760例患者符合条件,其中S组350例(12.7%),RT+S组2410例(87.3%)。简而言之,RT+S组男性比例、CEA升高、LND<12、T3均高于S组(all p <0.05)。而RT+S组肿瘤分化分级III/IV、TD、PNI、III期、N1/2率均低于S组(all p <0.05)。然而,经过1:1倾向性评分匹配后两组间的基线特征具有可比性(all p ≥ 0.05)。
PSM前,RT+S和S组的1,3,和4年CSS分别为98.02%vs.95.78%(p=0.078);90.63%vs.87.51%(p=0.224)和84.57%vs.82.94%(p=0.374)。PSM后,RT+S和S组的1,3,和4年CSS分别为97.94% vs. 96.27%(p= P=0.203); 93.58%vs.88.64%(p = 0.134)和88.36% vs. 83.68%(p = 0.279)。PSM前后都没有统计学差异。
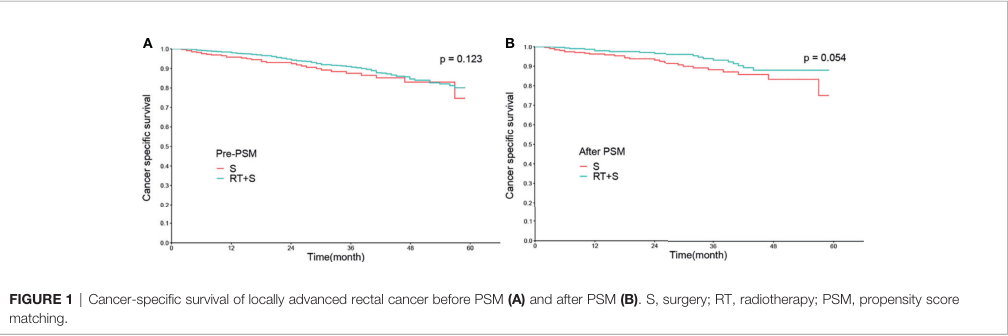
PSM前后的CSS
PSM前,两组的1,3和4年CSM分别为1.97% vs. 4.20% ( p = 0.068); 9.21% vs. 12.28% ( p = 0.189); 15.03% vs.16.61% ( p=0.364)。PSM后,两组的1,3和4年CSM分别为2.05%vs.3.72% (p=0.194); 6.38%vs.11.18% (p=0.110); 11.53% vs. 15.88% (p = 0.255)。PSM前后都没有统计学差异。
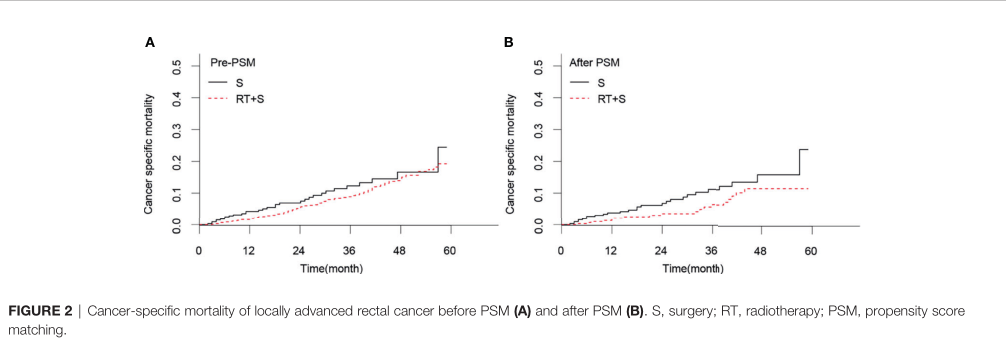
PSM前后的CSM
在匹配队列中,420例患者CEA水平正常,其中S组213例,RT+S组207例。在基线特征上,S组和RT+S组之间没有显著差异(all p≥0.05)。K-M生存分析显示,两组间中位CSS差异无统计学意义(HR = 0.73, 95% CI = 0.30 1.77, p = 0.490)。在CSM中也发现了类似的结果(HR = 0.74, 95% CI = 0.31 1.78, p = 0.500)。
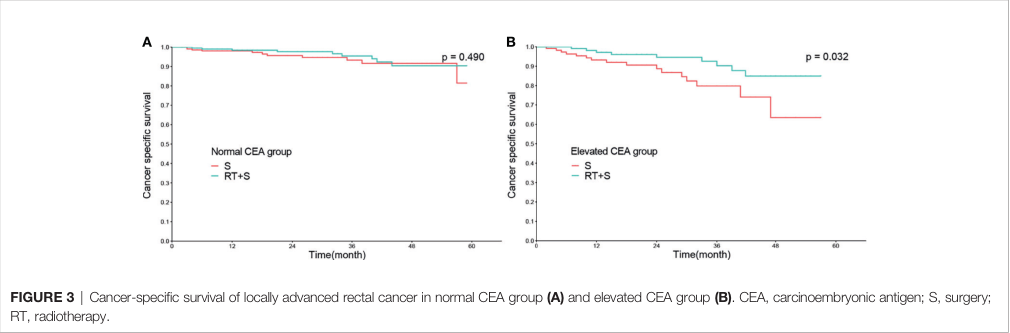
PSM后CEA水平对于CSS影响
在匹配队列中,242例患者在治疗前CEA水平升高,其中S组118例,RT+S组124例。同样,在基线特征方面,S组和RT+S组之间没有观察到显著差异(all p ≥0.05)。RT + S组的中位CSS优于S组(HR = 0.41, 95% CI 0.92 = 0.18, p = 0.032), 同样1,3和4年的CSS率也高于S组(97.12% vs 93.22%、90.24% vs 79.79%和84.91% vs 63.51%)。类似的,RT + S组的中位CSM优于S组(HR = 0.42, 95% CI = 0.19-0.94, p = 0.032;图4 b)。
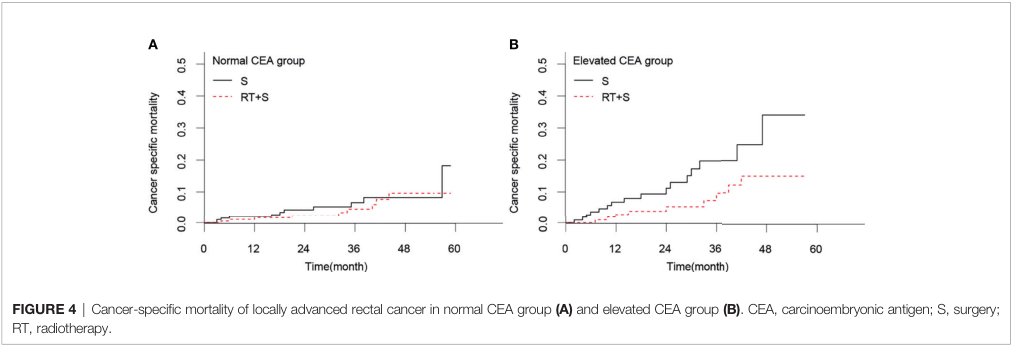
PSM后CEA水平对于CSM影响
此外,CEA升高亚组的多因素分析显示,术前放疗是CSS和CSM的独立保护因素(CSS: HR = 0.36, 95% CI = 0.15 0.83, p = 0.017;CSM: HR = 0.41, 95% CI = 0.18 0.94, p = 0.036)。
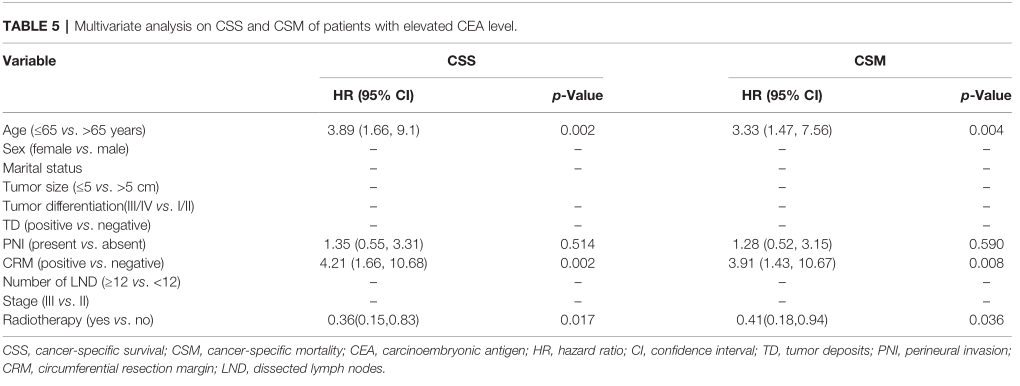
CEA升高患者CSS、CSM相关因素
综上,研究表明,治疗前CEA水平被认为是一个潜在的标志物,用于筛查从术前放疗获得长期生存的LARC患者。
原始出处:
Wang L, Zhong X, Lin H, Shao L, Chen G and Wu J (2021) The Correlation Between Survival Benefit of Preoperative Radiotherapy and Pretreatment Carcinoembryonic Antigen Level in Locally Advanced Rectal Cancer. Front. Oncol. 11:735882. doi: 10.3389/fonc.2021.735882
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者预后#
34
#局部晚期#
32
#局部晚期直肠癌#
26
#Oncol#
23
#局部#
27
#CEA#
35
放疗效果很好
54