Eur Heart J:Ciraparantag能逆转阿哌沙班和利伐沙班的抗凝血活性
2022-05-04 sunshine MedSci原创
Ciraparantag是一种抗凝剂(包括直接口服抗凝剂)的逆转剂。两项随机、安慰剂对照、剂量范围试验评估了ciraparantag逆转阿哌沙班或利伐沙班在健康老年人中诱导的抗凝治疗的疗效和安全性。
Ciraparantag是一种抗凝剂(包括直接口服抗凝剂)的逆转剂。近日,两项随机、安慰剂对照、剂量范围试验评估了ciraparantag逆转阿哌沙班或利伐沙班在健康老年人中诱导的抗凝治疗的疗效和安全性,研究结果已发表于Eur Heart J。
研究纳入120名50-75岁健康受试者,接受阿哌沙班(研究1)10 mg口服,每日两次,持续3.5天或利伐沙班(研究2)20 mg口服,每日一次,持续3天。充分抗凝后,受试者以3:1的比例随机分配到单次静脉注射剂量的ciraparatag组(研究1中,30、60或120 mg;研究2中,30、60、120或180 mg)或安慰剂组。疗效基于24小时内多个时间点的全血凝固时间(WBCT)校正。
结果显示,WBCT在给药后1小时内完全逆转,阿哌沙班组持续5小时或利伐沙班组持续6小时,与剂量相关。研究1中,ciraparatag 30mg,60mg,120mg和安慰剂组分别有67%、100%、100%和17%的受试者观察到逆转;研究2中,ciraparatag 30mg,60mg,120mg,180mg或安慰剂组分别有58%、75%、67%、100%和13%的受试者观察到逆转。安全性方面,研究发现与ciraparantag相关的不良事件是轻度、短暂的潮热或潮红。
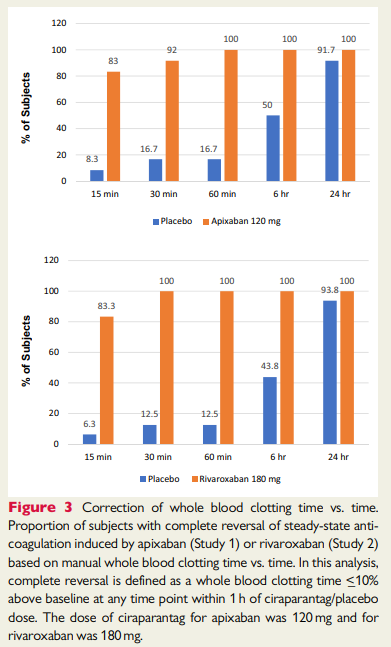
综上所述,该研究结果表明,ciraparantag与阿哌沙班或利伐沙班的稳态给药诱导的抗凝治疗呈剂量相关的逆转。阿哌沙班抗凝后使用60 mg ciraparantag,利伐沙班抗凝后使用180 mg ciraparantag可实现持续逆转。受试者对所有剂量的ciraparantag耐受性良好。
原始出处:
Jack Ansell, et al., Ciraparantag reverses the anticoagulant activity of apixaban and rivaroxaban in healthy elderly subjects. Eur Heart J. 2022 Mar 7;43(10):985-992. doi: 10.1093/eurheartj/ehab637.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#APA#
51
#ART#
35
#HEART#
44
学习了
62
太好了
60