Lancet Neurology:急性缺血性卒中(BP-TARGET)血管内治疗成功后强化降压的安全性和有效性:一项多中心、开放标签、随机对照试验
2021-04-07 MedSci原创 MedSci原创
急性缺血性卒中的血管内治疗显示出巨大的疗效,再灌注率超过80%。尽管有这种疗效,但超过一半的患者不能达到功能独立。
急性缺血性卒中的血管内治疗显示出巨大的疗效,再灌注率超过80%。尽管有这种疗效,但超过一半的患者不能达到功能独立。急性缺血性卒中研究的最大挑战现在不只是再灌注,还包括缺血再灌注损伤,包括血脑屏障破坏、脑水肿和脑实质内出血。急性缺血性卒中血管内治疗成功后的高收缩压与脑实质内出血风险增加有关。本研究旨在评估与标准收缩压相比,强化收缩压是否能降低脑实质内出血的发生率。
本研究是在法国进行的一项多中心、开放标签、随机对照试验。符合条件的个体为成年人(年龄≥18岁),其因大血管闭塞而发生急性缺血性中并通过血管内治疗获得成功。患者被随机分配(1:1)到强化收缩压组(100-129 mm Hg)或标准治疗收缩压组(130-185 mm Hg)。在两组中,目标收缩压必须在随机分组后1小时内达到,并通过静脉降压治疗维持24小时。主要终点是在24-36小时的影像学脑实质内出血,主要安全性终点是低血压的发生。
在2017年6月21日至2019年9月27日期间,四个参与卒中中心共招募了324名患者:162名患者被随机分配到强化目标组,162名患者被分配到标准目标组。再灌注后第一个24小时的平均收缩压在强化目标组为128mmHg (SD 11),在标准目标组为138mmHg(SD 11)。
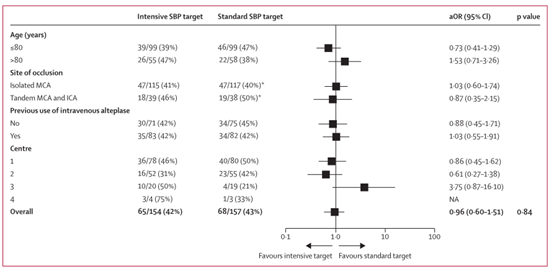
治疗效果对主要结果的影响
在再灌注后24-36小时内,在脑CT上观察到强化目标组154名患者中的65名(42%)和标准目标组157名患者中的68名(43%)的主要结果(调整后的比值比为0.96,95%CI 0.60-1.51;p=0.84)。两组间低血压事件无显著差异,强化目标组158例患者中有12例(8%)发生低血压事件,标准目标组160例患者中有5例(3%)发生低血压事件。随机分组后第一周内,强化目标组158例患者中有11例(7%)死亡,标准目标组160例患者中有7例(4%)死亡。
与标准治疗收缩压目标相比,本文的结果没有证据表明血管内治疗成功后急性缺血性卒中患者在24-36小时内将收缩压降低到100-129mmHg的强化策略对减少影像学实质内出血有任何影响。
Mazighi, MikaelMazighi, Mikael et al. Safety and efficacy of intensive blood pressure lowering after successful endovascular therapy in acute ischaemic stroke (BP-TARGET): a multicentre, open-label, randomised controlled trial. The Lancet Neurology, Volume 20, Issue 4, 265 - 274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Neurol#
39
#缺血性卒#
40
#对照试验#
42
#安全性和有效性#
39
#Lancet#
41
#target#
50
#多中心#
0
#对照#
39
#缺血性#
35
#强化降压#
53