Eur Urol Focus:如何减少前列腺癌患者在机器人辅助根治性前列腺切除术后的并发症风险?
2021-05-15 AlexYang MedSci原创
尽管以前的研究报告称,在机器人辅助前列腺根治术(RARP)治疗后,无论是否进行盆腔淋巴结清扫术(PLND),围手术期的效果都很好。而只有前瞻性地收集术后数据,才能真正了解手术效果情况。例如,近期的调查
尽管以前的研究报告称,在机器人辅助前列腺根治术(RARP)治疗后,无论是否进行盆腔淋巴结清扫术(PLND),围手术期的效果都很好。而只有前瞻性地收集术后数据,才能真正了解手术效果情况。例如,近期的调查表明,当进行一个前瞻性的系统数据收集系统时,RARP术后3个随访期间,报告的并发症发生率可高达30%。

前瞻性地收集围手术期结果数据,可能会提高对接受机器人辅助根治性前列腺切除术(RARP)前列腺癌(PCa)患者的手术结果的认识,也会促进实施旨在减少副作用风险的措施。
近期,研究人员评估了RARP术后最常见并发症的审计和反馈程序的有效性,以及为了改善结果采取的措施的有效性。
研究包括了415名RARP治疗的患者。根据欧洲泌尿外科协会的指南建议(第1组),研究人员前瞻性地收集了2016年9月至2017年12月期间接受治疗的187名患者的围手术期结果(30天)。2018年1月实施了审计和反馈程序,并据此确定了最常见的并发症,并实施了旨在改善结果的措施。之后研究人员将第1组的结果与实施改良手术技术的228名患者(第2组)的结果进行了比较。
研究人员在手术过程中采用了一种新的后部重建和尿道膀胱吻合术。围手术期结果包括失血量、手术时间、住院时间和术后30天的并发症。Logistic回归模型测试了新型手术技术对吻合口渗漏的影响。研究结果表明,97名患者(23%)在术后30天内出现了并发症。与第一组相比,第二组的吻合口渗漏率明显较低(3.1% vs 9.6%;P<0.01)。与第1组相比,第二组总的和Clavien-Dindo级≥2级的并发症发生率较低(17% vs 31%,6% vs 20%;均为p≤0.001)。在多变量分析中,实施吻合技术改良后的治疗可独立预测较低的并发症风险(OR 0.58,95%CI 0.38-0.89)和吻合口渗漏风险(OR 0.43,95% CI 0.17-0.97)。研究的主要局限性为缺乏随机化。
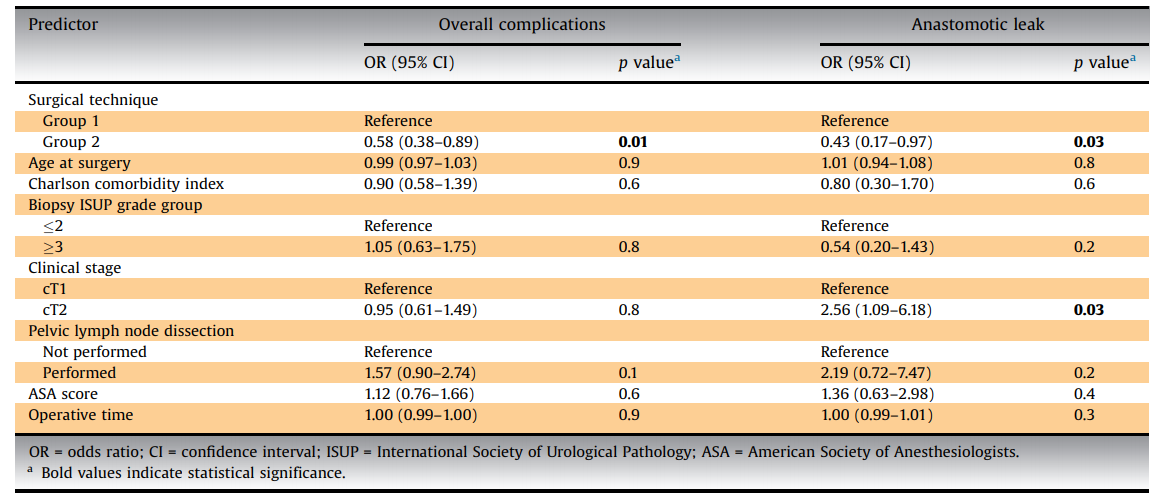
多变量逻辑回归模型预测总并发症和吻合口渗漏风险
他们的研究指出了对手术结果的认识的提高可促进尿道膀胱吻合技术的改良,进而减少吻合口渗漏的风险。他们的发现强调了使用标准化方法审计和反馈,进而报告手术的发病率是很有意义的。
原始出处:
Giuseppe Rosiello , Giorgio Gandaglia , Simone Scuderi et al. Reducing the Risk of Postoperative Complications After Robot-assisted Radical Prostatectomy in Prostate Cancer Patients: Results of an Audit and Feedback Intervention Following the Implementation of Prospective Data Collection. Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
37
#并发#
39
#前列腺切除#
35
#机器人#
38
#机器人辅助#
51
#机器#
29
#根治#
32
前列腺癌相关研究,学习了,谢谢梅斯
49