Hepatology:婴儿期含糖饮料的摄入量与学龄期肝脂肪积累之间存在相关性
2021-04-09 MedSci原创 MedSci原创
人在整个一生中,高糖饮食都是肥胖的重要危险因素。在一项关于成人的研究表明,摄入较多含糖饮料不仅与一般的肥胖有关,但也与增加肝内脂肪堆积相关。
人在整个一生中,高糖饮食都是肥胖的重要危险因素。在一项关于成人的研究表明,摄入较多含糖饮料不仅与一般的肥胖有关,但也与增加肝内脂肪堆积相关。增加的肝脂肪蓄积会导致的非酒精性脂肪肝病(NAFLD)是指一系列疾病的总称,包括肝脂肪变性到脂肪性肝炎,纤维化,肝硬化,最后是终末期肝病。最近有研究表明含糖饮料的摄入是儿童和成年人肥胖的主要危险因素,并且似乎与成年人的NAFLD有关。因此,本项研究旨在探究学龄儿童中婴儿期含糖饮料摄入量与肝脂肪蓄积和NAFLD之间的关系。
研究人员对1940名婴儿进行了前瞻性的研究,通过一项经过验证的食物频率问卷收集了所有患儿1岁时含糖饮料的摄入量。用核磁共振扫描(MR)评估患儿的肝脂肪分数和NAFLD(肝脂肪分数≥5.0%)发生率。
研究结果发现婴儿期含糖饮料摄入量较高与10岁时肝脂肪蓄积的增加无关 (P = 0.38)。但是,与每天<1.0份含糖饮料/天的婴儿相比,每天> 2.0份/天的婴儿在10岁时发生NAFLD的几率最高(OR,3.02; 95%CI,1.34,6.83)。在对学龄儿童的含糖饮料摄入量和体重指数进行进一步调整后,这些关联仍然处于临界状态(P = 0.13)。分层分析显示,受教育程度较低的母亲(OR,1.48; 95%CI,1.12,1.97)和超重或肥胖的儿童(OR,1.47; 95%CI,1.05,2.07)婴儿期含糖饮料摄入量与10岁以下的NAFLD之间存在更强的关联性。
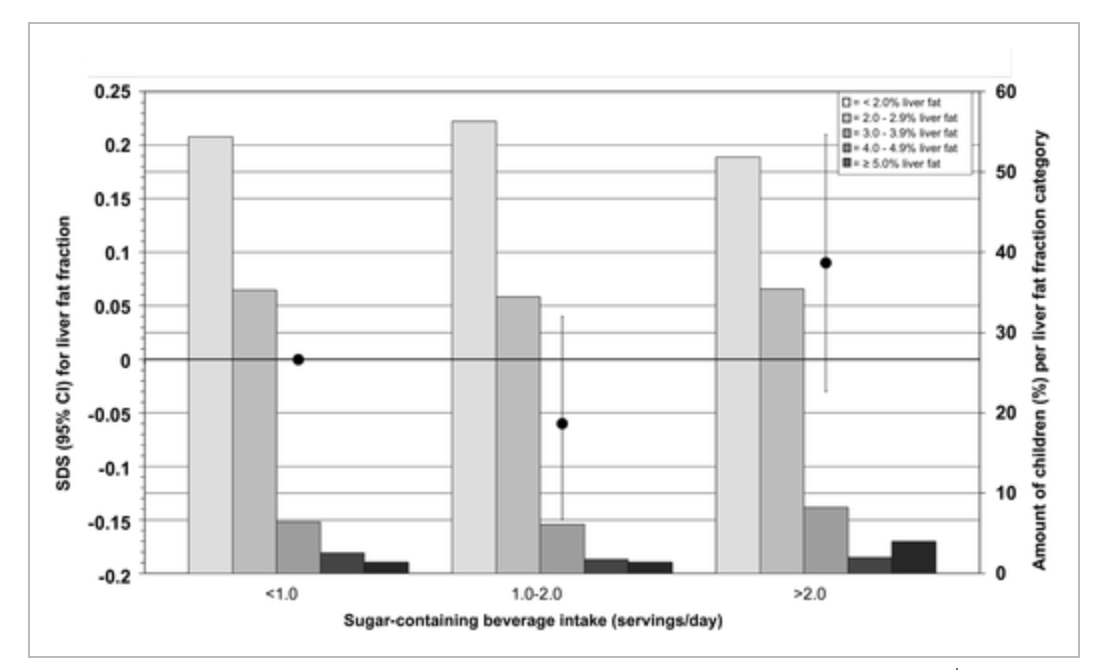
图:体重与肝脂肪累计的关系
本项研究证实婴儿期含糖饮料摄入量较高与学龄儿童的NAFLD相关,但与学龄期含糖饮料摄入量和体重指数无关。限制婴儿期含糖饮料的摄入可能有助于防止学龄期肝脂肪变性的发生。
原始出处:
Madelon L. Geurtsen. Et al. Associations Between Intake of Sugar‐Containing Beverages in Infancy With Liver Fat Accumulation at School Age. Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
41
#摄入量#
32
#EPA#
32
#婴儿期#
37
有帮助
53
感谢好文!
46