男子血压升高4年没找病因,结果突发胸痛伴撕裂感急诊!
2018-06-13 高进平、CC 医学界心血管频道
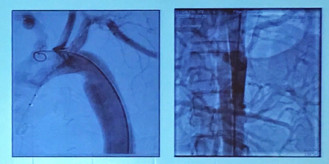
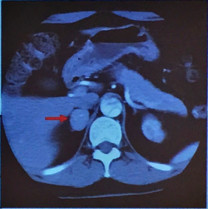
4年前体检测血压180/120mmHg,换用各种不同降压方案,血压始终重度升高。“突发胸痛伴撕裂感7小时”到我院急诊就诊。高血压急诊、CTA提示为降主动脉夹层。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#突发胸痛#
41
#血压升高#
34
学习了
73
好文献学习了
73
^_^^_^^_^
1