JAHA:美式足球运动员高血压和心室-动脉解偶联的患病情况
2022-02-26 MedSci原创 MedSci原创
VA解偶联与大学美式足球运动员的SBP病理性增加和左心室收缩功能的亚临床损伤相关,是该人群中观察到的不良心血管疾病表型的关键机制。未来的研究有必要分析针对性的临床干预是否可以改善VA耦合和健康结局。
心室-动脉(VA)耦合定义为动脉弹性(EA)与左心室弹性(ELV)之间的比率。VA解偶联,如发生在高血压性心脏病中,与患者不良结局相关。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在明确美式足球相关高血压与VA解偶联之间的关系。

这是一项针对参与3年美式足球运动的大学美式足球运动员进行的多中心、纵向和重复测量的观察性研究。在最初注册的200名新生运动员中,142名(67名黑人[47%]/75名白人[53%],58名前锋[41%]/84名非前锋[59%])接受了超声心动图和压平眼压计检查。该研究的主要超声心动图VA耦合结果指标包括EA/ELV和ΔEA/ELV,其中EA/ELV增加表明VA解耦。
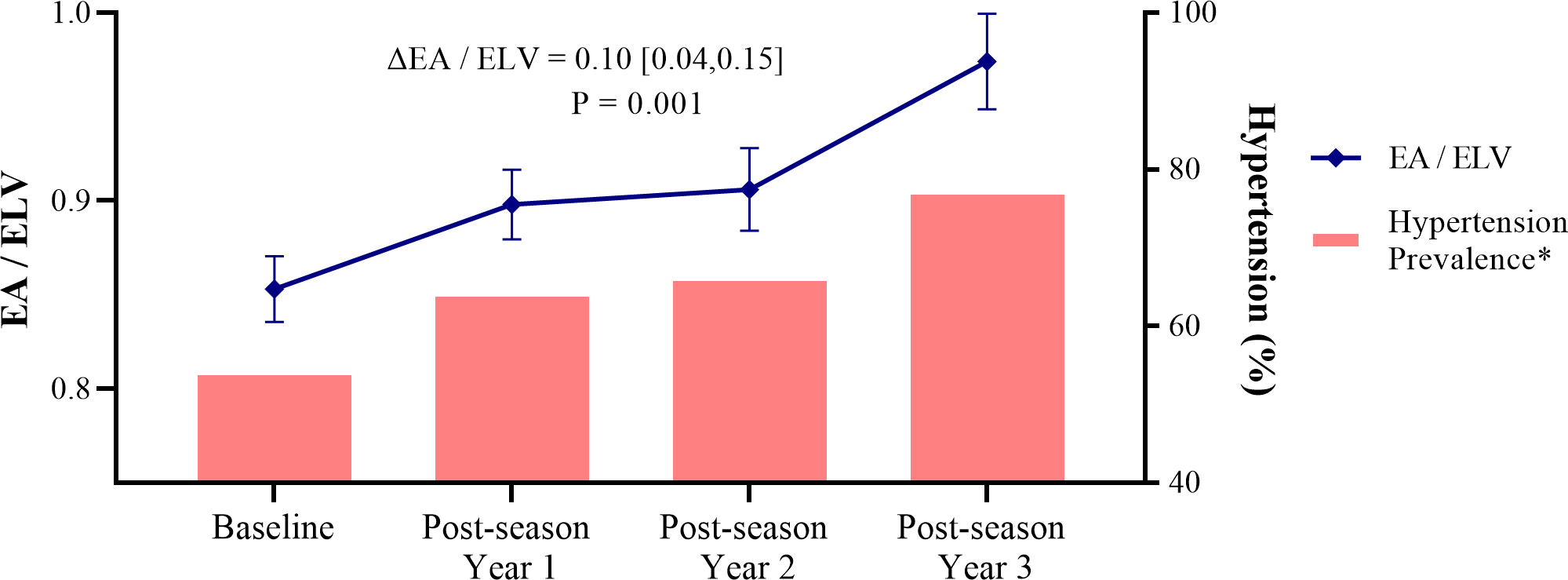
调整种族和球员位置后,美式足球运动员的EA/ELV(平均[95%CI]Δ为0.10[0.04-0.15];P=0.001)和收缩压(SBP)(平均[95%CI]Δ为11.4[8.3-14.5]mmHg,P<0.001)在他们的大学美式足球运动生涯中逐渐增加。结合纵向VA解偶联,高血压患病率(包括1期和2期高血压)从基线时的54%增加到研究期结束时的77%(2期高血压为44%)(P<0.001)。在多变量混合效应线性回归分析中,较高的SBP(β=0.021,P=0.02)、较低的E'(β=-0.010,P=0.03)和较差的整体纵向应变(β=0.036,P<0.001)与更高的EA/ELV相关。SBP增加(ΔSBP,β=0.029,P=0.02)和整体纵向应变恶化(Δ整体纵向应变,β=0.045,P<0.001)也预测ΔEA/ELV的增加。
由此可见,VA解偶联与大学美式足球运动员的SBP病理性增加和左心室收缩功能的亚临床损伤相关,是该人群中观察到的不良心血管疾病表型的关键机制。未来的研究有必要分析针对性的临床干预是否可以改善VA耦合和健康结局。
原始出处:
Jason V. Tso.et al.Hypertension and Ventricular–Arterial Uncoupling in Collegiate American Football Athletes.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.023430
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#病情#
47
#AHA#
53
#运动员#
46
学习了
60
学习
53
文章很实用
41
学习了
51
认真学习了
52