AACR重磅之KEYNOTE-042:帕博丽珠单抗持续延长了中国晚期/转移性PD-L1阳性NSCLC患者的生存期——Keynote-042中国研究的4年随访数据结果
2022-04-10 网络 网络
一线帕博丽珠单抗继续延长了中国晚期/转移性PD-L1阳性NSCLC患者的OS,并在随访近4年后提供了持久的反应。
在全球3期KEYNOTE-042研究中,帕博丽珠单抗(pembro)显著延长了先前未经治疗的晚期/转移性NSCLC患者(pts)的OS,这些患者的PD-L1 TPS≥1%,没有EGFR/ALK改变。
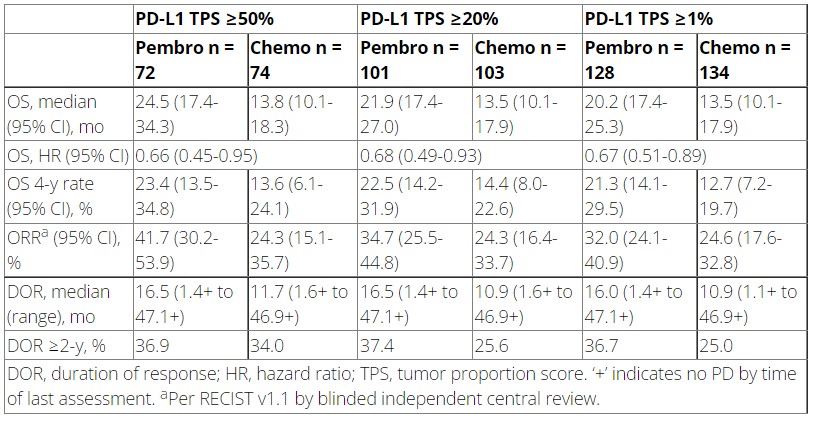
在中国入组的患者中,对于PD-L1 TPS≥50%(HR=0.63;95%CI 0.43-0.94)、TPS≥20%(0.66;0.47-0.92)和TPS≥1%(0.67;0.50-0.89)的患者,与化疗相比,帕博丽珠单抗延长了OS的结果。
近期,在AACR2022大会上,来自广东省人民医院吴一龙教授介绍了KEYNOTE-042中中国患者继续随访14个月的疗效和安全性结果。

参加KEYNOTE-042全球研究(NCT02220894)和中国扩展研究(NCT03850444)的入组的患者按1:1的比例随机选择帕博丽珠单抗(200 mg Q3W,持续≤35个周期)或卡铂+紫杉醇/培美曲塞(非鳞癌患者可选择培美曲塞维持治疗)。主要终点是PD-L1 TPS≥50%、≥20%和≥1%的患者的OS。符合条件的患者在完成了35个周期的培美曲塞后可以接受第二个疗程的培美曲塞。
结果显示,262名PD-L1 TPS≥1%的患者在中国被随机分配到帕博丽珠单抗(n = 128)或化疗(n = 134)。从随机入组到数据截止(2021年4月28日)的中位时间是47.2(范围,39.8-56.1)月。总的来说,与化疗相比,帕博丽珠单抗延长了PD-L1 TPS≥50%(0.66,0.45-0.95)、≥20%(0.68,0.49-0.93)和≥1%(0.67,0.51-0.89)患者的OS。
帕博丽珠单抗组和化疗组分别有19.5%和68.8%的患者出现了治疗相关的3-5级副作用。在22名完成35个周期帕博丽珠单抗治疗的患者中,ORR为81.8%(95%CI,59.7%-94.8%);随机后4年的估计OS率为69.1%。
该研究显示,与全球KEYNOTE-042研究相似,一线帕博丽珠单抗继续延长了中国晚期/转移性PD-L1阳性NSCLC患者的OS,并在随访近4年后提供了持久的反应。可见帕博丽珠单抗单药治疗仍然是这些患者的标准疗法。
来源:
https://www.abstractsonline.com/pp8/#!/10517/presentation/20294
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#阳性NSCLC#
44
#SCLC患者#
42
#KEYNOTE#
49
#PD-L1#
44
#生存期#
46
#转移性#
47
#ACR#
43
#PD-L1阳性#
50
#NSCLC患者#
35
#重磅#
44