Behavioural Brain Research:重性抑郁症患者缓解期认知功能网络改变的独立成分分析
2020-12-23 MedSci原创 MedSci原创
在抑郁症患者中观察到静息状态功能网络的功能障碍性连接性,尤其是在包括中枢执行网络(CEN)、默认模式网络(DMN)和凸显网络(SN)的认知功能网络中。神经心理学研究报告称,缓解型MDD患者存在认知功能
在抑郁症患者中观察到静息状态功能网络的功能障碍性连接性,尤其是在包括中枢执行网络(CEN)、默认模式网络(DMN)和凸显网络(SN)的认知功能网络中。神经心理学研究报告称,缓解型MDD患者存在认知功能障碍(处理速度和执行功能)。认知功能障碍一直是预测MDD患者使用选择性5-羟色胺再摄取抑制剂(SSRIs)治疗后功能恢复的一个关键因素。抗抑郁药物(ADM)对MDD的影响仍然没有得到充分的认识和治疗。三个核心网络内部和跨三个核心网络的异常连接模式已经在初次用药的MDD患者中得到证实。使用SSRI治疗,完全恢复是可能的,尤其是在认知功能方面,但不完全恢复是常见的。然而,从研究抗抑郁药治疗后异常功能连接(FC)的变化来看,结果并不一致。因此,本研究旨在探讨缓解型重性抑郁障碍(rMDD)患者与健康对照者(HCs)静息状态下认知功能网络改变的潜在机制,并进一步探讨rMDD的功能障碍连接模式与临床症状之间的关系。
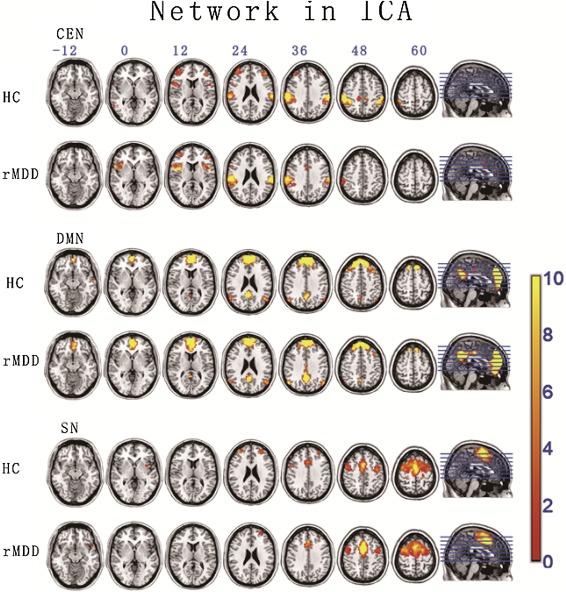
在这项研究中,19名HCs和19名rMDD患者接受静息状态功能磁共振成像(fMRI)扫描。使用梯度回忆回波平面成像(GRE-EPI)脉冲序列横向采集静息状态功能图像,设置如下:重复时间(TR)/回波时间(TE)=3000 ms/40 ms,切片厚度=4.00 mm,矩阵尺寸=64×64,翻转角度=90°,视野(FOV)=240 mm×240 mm。每个受试者扫描持续5.06分钟。每个受试者均获得T1加权磁化制备梯度回波(MPRAGE)图像,进行空间归一化和定位。采用CEN、DMN和SN的独立成分分析评价FC。进行了两个样本t检验来比较rMDD和HCs之间的差异。此外, 还进行了Pearson相关分析,以检验网络连通性与认知功能评分和临床症状之间的关系。
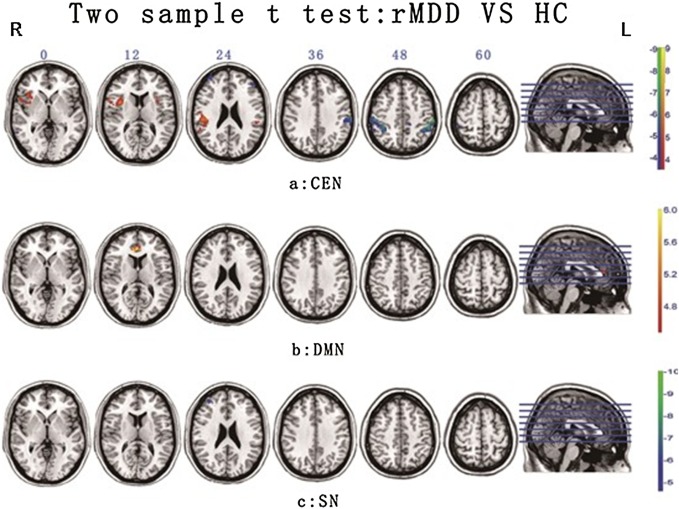
与健康对照组相比,缓解期患者的CEN连接性较低,主要位于额上回(SFG)、额中回(MFG)、顶叶下叶(IPL)和部分边缘上回(SMG)。相反,rMDD患者双侧岛叶、部分SMG(CEN的关键节点)和DMN的背侧前扣带回皮质(dACC)显示出更高的连通性。Pearson相关分析结果表明,CEN右侧IPL的连通性与认知功能评分呈正相关,而左侧岛叶的连通性与BDI评分呈负相关。 尽管在先前的研究中,部分位于CEN和SN的DLPFC和IPL的额头顶叶关键节点的连接性持续降低表明MDD患者的认知控制低于HCs,但在本研究中,这可能是残余认知症状和复发风险的预测因子。位于CEN额叶外层深层的ACC(包括dACC)的高活性可能在认知功能的恢复中起关键作用。 研究结果强调了大脑额叶和顶叶的关键认知控制和恢复机制的可能性。
rMDD患者虽然达到临床缓解标准,但其认知功能网络仍存在独特的功能损害。在rMDD中观察到负责执行控制的认知功能网络之间的异常FC,这种现象可能与临床症状有关。
Liu, G., et al., The alteration of cognitive function networks in remitted patients with major depressive disorder: an independent component analysis. Behavioural Brain Research, 2021. 400: p. 113018.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抑郁症患者#
0
#缓解期#
29
#HAV#
32
#EHA#
32
#Research#
37
学习了
65
每天学习一点点
84
学习了,谢谢分享
63