Dig Dis Sci:布拉氏酵母菌联合甲硝唑可有效治疗系统性硬化症患者的SIBO
2020-12-06 MedSci原创 MedSci原创
高达60%的系统性硬化症(SSc)患者存在小肠细菌过度生长(SIBO),使用抗生素后这些患者会有所改善。此外,添加益生菌可以带来更好的效果。一项临床试验评估了布拉氏酵母菌(SB)VS. 甲硝唑(M)V
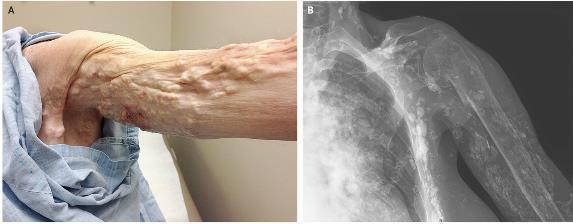
高达60%的系统性硬化症(SSc)患者存在小肠细菌过度生长(SIBO),使用抗生素后这些患者会有所改善。此外,添加益生菌可以带来更好的效果。一项临床试验评估了布拉氏酵母菌(SB)VS. 甲硝唑(M)VS. M+SB治疗2个月在SSc中减少胃肠道症状和SIBO的疗效和安全性,研究结果已在线发表于Dig Dis Sci。

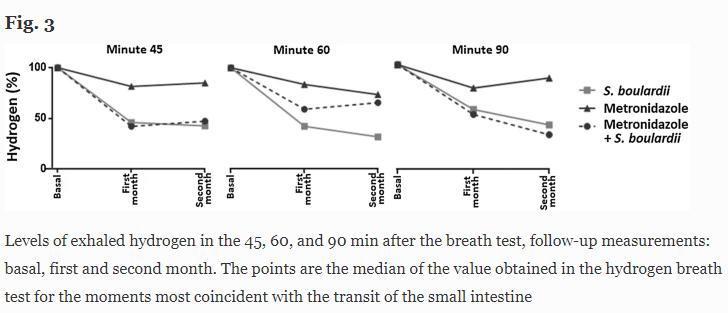
研究纳入了40名SIBO和SSc(ACR-EULAR 2013)患者,分配了三组:M、SB和M+SB,为期2个月。使用氢气呼气试验测量氢气的百万分之几,以评估SIBO。应用美国国立卫生研究院患者报告的结果测量信息系统(NIH-PROMIS)问卷量化胃肠道症状。
结果显示,组间基线特征相似。平均年龄为53.2±9.3岁,SSc的演变过程为13.5(1-34)年。治疗2个月后,M+SB组55%的SIBO被根除。SB组和M+SB组的腹泻、腹痛、气胀/腹胀减少,但M组保持不变。45~60min时氢气排出减少的情况如下:第一个月和第二个月时,M+SB分别为48%和44%,M为18%和20%,SB为53%和60%(P<0.01)。不良反应方面,M(53%)和M+SB(36%)出现上腹灼热和便秘,SB(22%)出现胀气/腹泻。
综上所述,该研究结果表明,甲硝唑治疗对SIBO部分有效,但布拉氏酵母菌单药或联合用药可改善SSc的胃肠道结果。
原始出处:
Grettel García-Collinot, Eduardo Osiris Madrigal-Santillán, et al., Effectiveness of Saccharomyces boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020 Apr;65(4):1134-1143. doi: 10.1007/s10620-019-05830-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#SIBO#
39
#Dis#
27
#硬化症#
38
#系统性#
28
#甲硝唑#
46
#有效治疗#
0
#系统性硬化#
30
学习了,谢谢分享
84