PLoS Med:肥胖和营养不良与心脏重构和心血管结局的相关性
2021-06-03 Nebula MedSci原创
肥胖是心血管疾病和心力衰竭(HF)众所周知的风险因素,与普通人群的不良心室重构相关。营养状况如何改变肥胖与相关健康预后之间的关系尚未完全明确。该研究旨在调查肥胖和营养状况与普通社区人群的临床特征、超声
肥胖是心血管疾病和心力衰竭(HF)众所周知的风险因素,与普通人群的不良心室重构相关。营养状况如何改变肥胖与相关健康预后之间的关系尚未完全明确。该研究旨在调查肥胖和营养状况与普通社区人群的临床特征、超声心动图变化和临床预后之间的相关性。
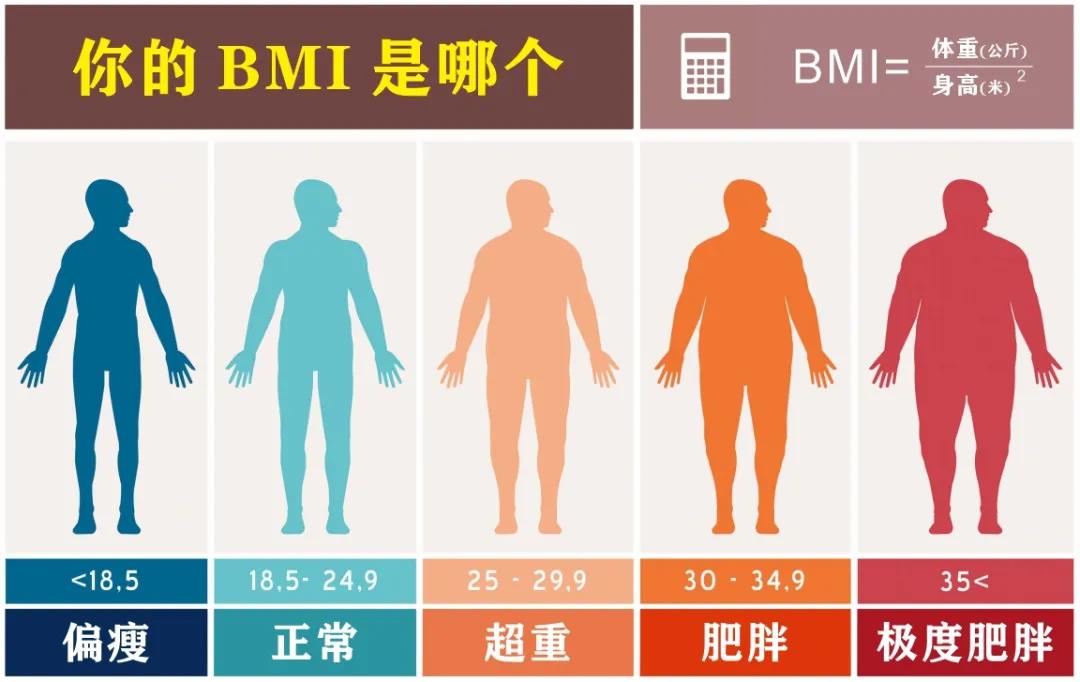
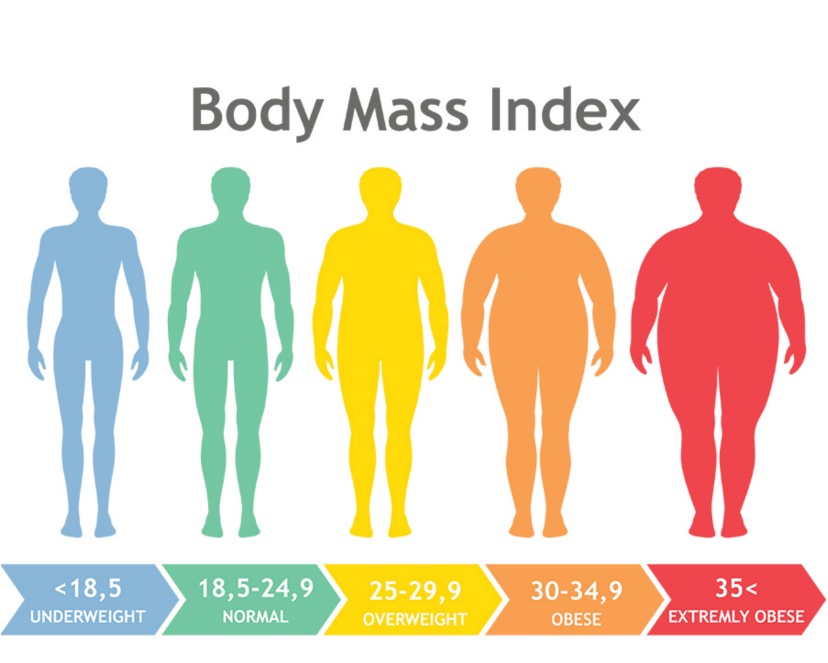
2009年6月-2012年12月期间,研究人员对前瞻性招募的5300名无症状的亚洲受试者(平均49.6±11.4岁,男性 64.8%)进行了心血管健康筛查。描述了受试者的临床和超声心动图特征,并根据肥胖和营养状况进行分层。以体重指数(BMI)界定肥胖(>25 kg/m2)。根据血清白蛋白(SA)浓度界定营养状况(低 <45 g/L[营养不良];高 ≥45 g/L[营养良好]),其次是预后营养指数(PNI)和全球营养不良领导倡议(GLIM)标准。采用Cox比例风险模型评估1年因心衰或全因死亡率住院的综合预后,同时根据年龄、性别和其他临床混杂因素进行校正。
该以社区为基础的队列分别包含2096位(39.0%)瘦-营养良好(低BMI,高SA)、1369位(25.8%)肥胖-营养良好(高BMI,高SA)、1154位(21.8%)瘦-营养不良(低BMI,低SA)和681位(12.8%)肥胖-营养不良(高BMI,低SA)的个体。
以BMI划分亚组的心衰住院和1年死亡率的复合结局
与其他所有亚组相比,肥胖-营养不良的受试者的平均年龄更大(54.5±11.4岁)、女性更常见(41%)、平均腰围(91.7±8.8 cm)更大、体脂比例最高(32%),高血压(32%)、糖尿病(12%)和心血管疾病史(11%)的发生率最高(均p<0.001)。
以腰围划分亚组的心衰住院和1年死亡率的复合结局
与营养良好组相比,营养不良组个体的N末端B型利钠肽前体(NT-proBNP)水平显著升高,瘦组(70.7±177.3 vs 36.8±40.4 pg/mL)和肥胖组(73.1±216.8 vs 33.2±40.8 pg/mL)水平相似(p<0.001)。
以体脂量划分亚组的心衰住院和1年死亡率的复合结局
与瘦-营养良好组(低BMI,高SA)及其他所有亚组相比,肥胖-营养不良组(高BMI,低SA)的左心室重构更明显(左心室质量指数为44.2±1.52 vs 33.8±8.28 gm/m2;相对心室壁厚度 0.39±0.05 vs 0.38±0.06),舒张功能较差(p<0.001)。
平均随访3.6年期间,肥胖-营养不良组的复合不良结果的多变量校正风险最高(危险比[HR] 2.49, 95%CI 1.43-4.34,p=0.001),其次是瘦-营养不良组(HR 1.78, 95%CI 1.04-3.04,p=0.034)和肥胖-营养良好(HR 1.41,95% CI 0.77-2.58, p=0.27)组(以瘦-营养良好组为参考)。
总而言之,该研究表明营养状况不佳的肥胖个体具有最高的合并症负担、最不利的心脏重构和最不利的复合结果。
原始出处:
Chien Shih-Chieh,Chandramouli Chanchal,Lo Chi-In et al. Associations of obesity and malnutrition with cardiac remodeling and cardiovascular outcomes in Asian adults: A cohort study.[J] .PLoS Med, 2021, 18: e1003661. https://doi.org/10.1371/journal.pmed.1003661
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#相关性#
48
学习了
75
#心血管结局#
54
#Med#
55
学习了
64
实用
67