ESC 2020:ACS患者LDL-C管理:低一些好一些,早一些好一些?!
2020-09-17 心关注 心关注
ESC 2020会议上,关于PCSK9抑制剂的专题会议分享了急性冠脉综合征(ACS)患者降脂治疗的最新研究结果,回顾并展望了ACS患者降脂治疗的历史数据和未来研究。
血脂异常是动脉粥样硬化性心血管疾病(ASCVD)的关键致病因素。FOURIER研究[1]按LDL-C水平进行分层发现,随着降脂治疗带来的LDL-C水平的进一步降低,心血管事件进一步下降,且安全性良好,未观察到以往所担心的认知功能障碍等不良反应,提示对ASCVD患者LDL-C低一些好一些。ESC 2020会议上,关于PCSK9抑制剂的专题会议分享了急性冠脉综合征(ACS)患者降脂治疗的最新研究结果,回顾并展望了ACS患者降脂治疗的历史数据和未来研究。《心关注》特邀哈尔滨医科大学附属第一医院副院长李悦教授分享会议精彩观点和重要信息,为临床医师制定ACS患者的血脂管理策略提供参考。
依洛尤单抗全面、显着提升ACS患者致动脉粥样硬化脂质指标达标率
LDL-C水平升高与Peri-ACS期和ACS后早期不良缺血性事件风险升高相关。然而高强度他汀治疗4周通常不能使LDL-C水平达到ESC和AHA/ACC对高危患者(如ACS患者)二级预防的推荐。PCSK9抑制剂为Peri-ACS期和ACS后早期患者降低LDL-C提供了一个额外、迅速、有效的选择。
EVACS研究[2]探讨了依洛尤单抗在ACS患者中的应用,研究共纳入57例肌钙蛋白Ⅰ≥5 ng/ml的非ST段抬高型心肌梗死(NSTEMI)患者,随机分配在就诊24小时内接受依洛尤单抗(n=30)或安慰剂(n=27)治疗组。组间除性别外,患者基线特征如年龄、体重指数(BMI)、糖尿病、高血压、既往他汀类药物治疗以及LDL-C水平(91.5 mg/dl vs. 89.6 mg/dl)等均无显着差异。对受试者个体数据采用线性混合效应模型,校正基线LDL-C水平、性别、降脂治疗、时间和中心后发现,依洛尤单抗组第1天LDL-C水平降低21.1 mg/dl,第3天即显着低于安慰剂组(49.2 mg/dl vs. 76.1 mg/dl,P=0.02),组间差异在住院期间以及随访30天内(P<0.01)持续存在。随访30天时,线性回归分析显示,校正基线LDL-C水平、他汀应用、他汀用药改变和依折麦布应用后,依洛尤单抗组平均LDL-C水平较安慰剂组显着降低28.6 mg/dl(P<0.0001);依洛尤单抗组non-HDL和apoB水平亦较安慰剂组显着降低。无论采用AHA/ACC指南还是ESC指南对ACS患者致动脉粥样硬化脂质的目标值推荐,依洛尤单抗均较安慰剂极大提高出院时LDL-C(<70 mg/dl:80.8% vs. 38.1% 和<55 mg/dl:65.4% vs. 23.8%,P均=0.01)、non-HDL和apoB的达标率;随访30天时,依洛尤单抗组各项脂质指标与安慰剂组相比在ESC目标值达标率方面仍存在显着差异(图2)。不良事件两组间未见显着差异。
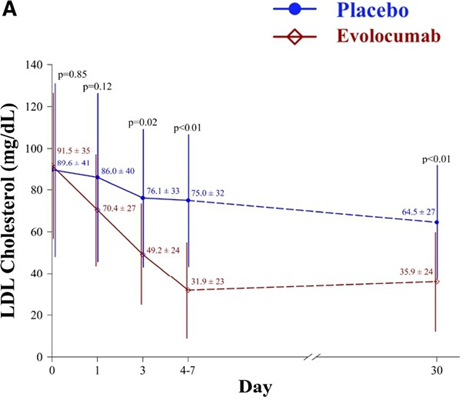
图1. 依洛尤单抗显着降低ACS患者LDL-C水平
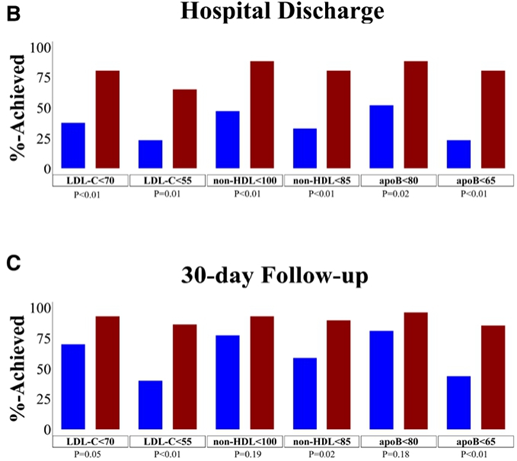
图2. 依洛尤单抗显着升高ACS患者LDL-C、non-HDL、和apoB达标率
ACS患者早期降脂干预的斑块影响将添新证据:依洛尤单抗HUYGENS研究
影像学从冠脉CT、MR血管造影、血管内超声-虚拟组织学(IVUS-VH)到光学相干断层扫描(OCT)的发展,不断推动我们对斑块的认识。对采用IVUS监测斑块进展的降脂治疗研究进行的荟萃分析证实,他汀治疗将LDL-C水平降至低于70 mg/dl可使动脉粥样硬化斑块发生逆转[3]。他汀治疗可以纠正更易进展、更易破裂、更易导致临床事件的高危斑块(斑块负担高、广泛血管重构、点状钙化),降低动脉粥样硬化体积百分比(PAV),逆转斑块进展[4]。GLAGOV研究证实,与单用他汀相比,加用依洛尤单抗可使冠状动脉疾病(CAD)患者的LDL-C从93 mg/dl进一步降低至36.6 mg/dl,实现显着的斑块逆转(PAV:依洛尤单抗组-0.95% vs. 安慰剂组+0.05%,P<0.001),且更大比例(64.3% vs. 47.3%)患者得以实现斑块逆转[5]。
OCT使我们能够定量降脂治疗带来的易损斑块变化,如纤维帽厚度、脂质池和巨噬细胞池大小。日本早期很多小规模研究提示,他汀治疗可以增加纤维帽厚度,提示了降脂治疗存在潜在的稳定斑块的作用。在接受最大耐受剂量他汀类药物治疗的非ST段抬高型ACS(NSTE-ACS)患者中,通过OCT监测探讨依洛尤单抗对纤维帽厚度影响的HUYGENS研究[6]目前正在进行中,结果有望在近期发布(图3)。

图3. 正在进行中的依洛尤单抗HUYGENS研究
小结:重视极高危患者群体联合降脂应用,推进指南走入现实
第一项评估PCSK9单克隆抗体在极高危ACS急性期应用的EVOPACS研究证实,对于LDL-C水平升高的ACS患者,在他汀治疗基础上院内开始加用依洛尤单抗治疗8周可以使90%以上(安慰剂组11%)患者达到最新ESC/EAS血脂异常指南推荐的LDL-C目标水平(LDL-C<1.4 mmol/L),且在研究期间依洛尤单抗的安全性和耐受性良好[7]。ESC 2020公布的日本研究证实,在接受直接PCI的AMI患者中,早期(PCI术后24小时内)应用依洛尤单抗同样可以迅速强效降低LDL-C水平,使高达95.9%的患者在4周内实现LDL-C<55 mg/dl[8]。EVACS研究规模虽小,但提供了新的重要依据,依洛尤单抗不仅显着降低LDL-C水平,同时明显降低致动脉粥样硬化的non-HDL和apoB水平,显着提高这些指标的达标率。同时,HUYGENS研究也将会为依洛尤单抗对ACS患者斑块稳定性的影响深入探索提供新证据,值得期待。这些研究会有助于我们更好地理解依洛尤单抗在ACS患者早期应用的获益机制,也会在LDL-C降得“低一些好一些”之外,为“早一些好一些”提供新的证据。截至目前,可以明确的是,对ACS患者急性期这种临床实践中的极高危情况,他汀联合依洛尤单抗为我们提供了一种非常有效且安全性良好的强化降脂策略,可使绝大多数患者快速实现致动脉粥样硬化脂质指标的全面达标,为患者更早、更多获益打下良好基础。
原始出处:
[1] Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017;390(10106):1962-1971.
[2] Leucker TM, Blaha MJ, Jones SR, et al. Effect of Evolocumab on Atherogenic Lipoproteins During the Peri- and Early Postinfarction Period: A Placebo-Controlled, Randomized Trial. Circulation. 2020;142(4):419-421.
[3]Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med. 2011;365(22):2078-2087.
[4] Kataoka Y, Wolski K, Balog C, et al. Progression of coronary atherosclerosis in stable patients with ultrasonic features of high-risk plaques. Eur Heart J Cardiovasc Imaging. 2014;15(9):1035-1041.
[5]Nicholls SJ, Puri R, Anderson T, et al. Effect of Evolocumab on Progression of Coronary Disease in Statin-Treated Patients: The GLAGOV Randomized Clinical Trial. JAMA. 2016;316(22):2373-2384.
[6] https://clinicaltrials.gov/ct2/show/NCT03570697.
[7]KC Koskinas et al.Evolocumab for Early Reduction of LDL Cholesterol Levels in Patients With AcuteCoronary Syndromes (EVOPACS). J Am Coll Cardiol 2019; 74 (20):2452-2462.
[8]Tomoaki Okada, et al. Feasibility and safety of early initiation of a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor in patients with acute myocardial infarction undergoing primary PCI. ESC Congress 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












低一些好一些,早一些好一些
96
#ACS#
37
#LDL#
35
#ACS患者#
46
好文章,学习了
103