Nat Med:多发性骨髓瘤患者在BCMA靶向CAR-T治疗后或引起BCMA纯合缺失
2021-02-24 xiaozeng MedSci原创
B细胞成熟抗原(BCMA)作为多种免疫疗法的靶点,也是多发性骨髓瘤(MM)中与肿瘤负荷相关的生物标志物。
B细胞成熟抗原(BCMA)作为多种免疫疗法的靶点,也是多发性骨髓瘤(MM)中与肿瘤负荷相关的生物标志物。BCMA的编码基因TNFRSF17位于16号染色体的短臂上,其几乎仅在浆细胞和B细胞上表达。
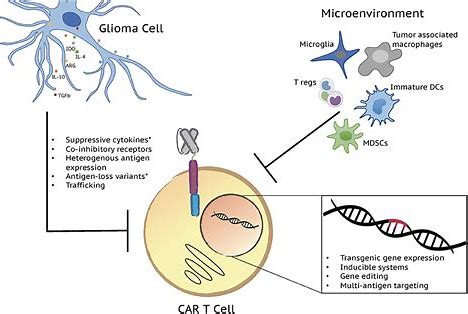
既往研究显示,MM患者血清中可溶性sBCMA的水平升高,且与疾病的发生相关。BCMA相关免疫疗法包括CAR(嵌合抗原受体)-T细胞疗法,其在复发性/难治性MM中显示出潜在的治疗活性。虽然目前已在少数患者中观察到BCMA抗原表达的降低或丧失,但仍未阐明BCMA靶向CAR-T细胞疗法复发的肿瘤内在机制。
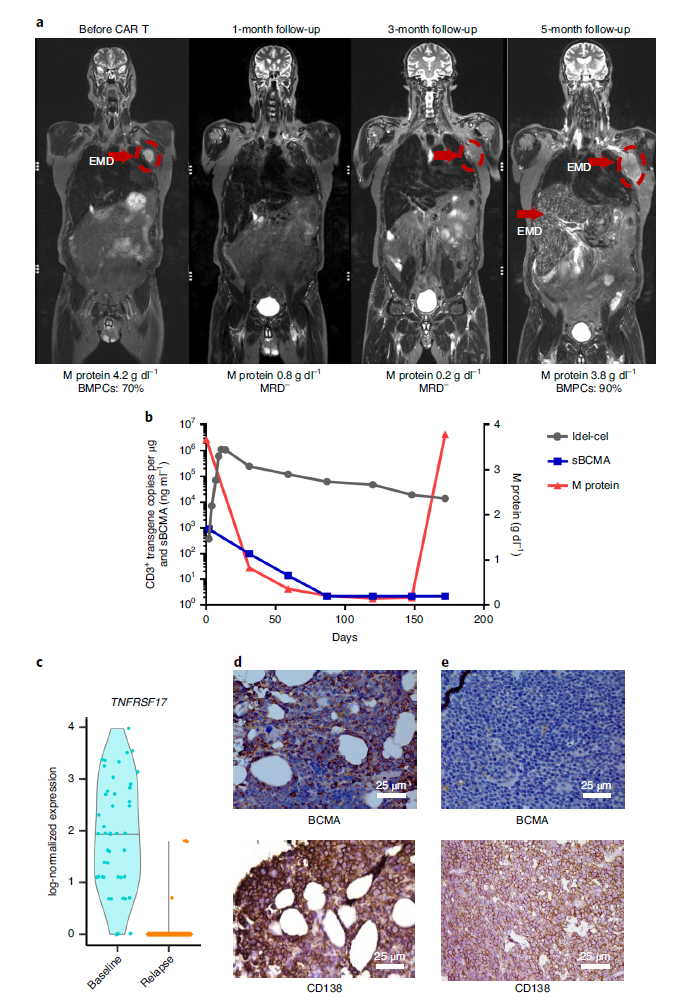
在该研究中,研究人员报告了一名参与KarMMa试验(NCT03361748)的携带BCMA不可逆缺失的MM患者,该患者在接受抗BCMA CAR-T治疗后出现了疾病的进展。
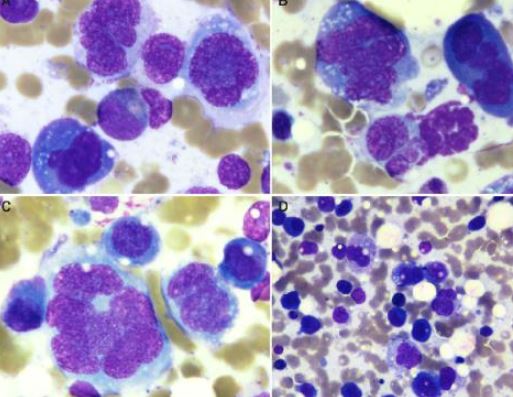
患者的临床特征和BCMA的表达情况
研究人员发现,TNFRSF17(BCMA)基因的纯合缺失是免疫逃逸的一个潜在机制。此外,进一步的研究显示,在168例MM患者中有37例出现了TNFRSF17杂合缺失或16号染色体部分缺失,其中,33例超单倍体MM患者中的28例先前并未接受BCMA靶向治疗,这说明从理论上而言,TNFRSF17杂合缺失可能是免疫治疗后BCMA缺失的一大危险因素。
总而言之,该研究揭示了CAR-T细胞治疗前后16号染色体畸变的罕见存在,这与影响TNFRSF17基因座以逃避BCMA靶向免疫疗法的基因组不稳定性有关。
原始出处:
Da Vià, M.C., Dietrich, O., Truger, M. et al. Homozygous BCMA gene deletion in response to anti-BCMA CAR T cells in a patient with multiple myeloma. Nat Med (22 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CAR-#
32
#Nat#
35
#多发性#
32
#BCMA#
47
#Med#
37