J Clin Endocrinol Metab:孕激素和睾酮联合注射可有效用于男性避孕
2016-10-28 MedSci MedSci原创
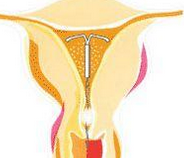
目前,仍未有一种安全有效的可逆性男性避孕方法。本研究旨在评估联用孕激素和睾酮注射抑制精子发生和避孕保护的效果。 采用前瞻性多中心研究设计,在十个研究中心,纳入18-45岁的健康男性,以及其18-38岁的女性伴侣,均无生育问题。 对男性参与者进行肌内注射庚酸炔诺酮200毫克和1000毫克睾酮,每8周给药一次。然后通过精液分析精子发生的抑制作用,通过妊娠率来评估避孕保护效果。 结果,
目前,仍未有一种安全有效的可逆性男性避孕方法。本研究旨在评估联用孕激素和睾酮注射抑制精子发生和避孕保护的效果。
采用前瞻性多中心研究设计,在十个研究中心,纳入18-45岁的健康男性,以及其18-38岁的女性伴侣,均无生育问题。
对男性参与者进行肌内注射庚酸炔诺酮200毫克和1000毫克睾酮,每8周给药一次。然后通过精液分析精子发生的抑制作用,通过妊娠率来评估避孕保护效果。
结果,在320名参与者中,95.9%的参与者(95%可信区间[CI],92.8-97.9)24周内精子浓度≤100万个/毫升。在长达56周的有效期内,266名男性参与者的伴侣仅有4名怀孕,怀孕率为 1.57%(95% CI,0.59-4.14)。52周后的抑制精子发生的累积可逆性恢复为94.8%(95% CI,91.5-97.1)。最常见的不良反应是痤疮、注射部位疼痛、性欲减退和情绪障碍。
该研究显示,联合孕激素和睾酮注射可近100%的抑制精子的发生,且效果可逆。与其他可供使用的男性可逆避孕方法相比,本研究所使用的方法避孕效果相对较好。但是该方法轻度至中度情绪障碍的频率相对较高。
原始出处:
Hermann M. Behre,et al., Efficacy and Safety of an Injectable Combination Hormonal Contraceptive for Men. Journal of Clinical Endocrinology & Metabolism, October 27, 2016 DOI: 10.1210/jc.2016-2141.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Meta#
39
#MET#
33
谢谢分享!
81
谢谢分享!
74
#孕激素#
42