Eur Urol:Avelumab联合SABR是否能促进转移去势抵抗性前列腺癌的疗效?
2021-09-23 AlexYang MedSci原创
评估了PD-L1抑制剂alvumab与立体定向消融体放疗(SABR)联用对mCRPC的疗效和安全性。
在过去的十年中,不断出现能够延长转移去势抵抗性前列腺癌(mCRPC)患者生命的疗法,包括第二代雄激素受体(AR)通路抑制剂、他汀类化疗药物卡巴他赛以及PARP抑制剂。相比之下,使用PD-1/PD-L1和CTLA-4抗体的免疫检查点抑制疗法,尽管在一系列的泌尿系统恶性肿瘤中发挥了作用,但益处不大。免疫抑制性的前列腺肿瘤微环境仍然是在临床治疗的一个重要障碍。

免疫检查点抑制剂对转移去势抵抗性前列腺癌(mCRPC)的治疗效果不大,但高剂量放疗可能与检查点抑制剂有协同作用。
近期,来自澳大利亚的研究人员在《Eur Urol》上发表文章,评估了PD-L1抑制剂alvumab与立体定向消融体放疗(SABR)联用对mCRPC的疗效和安全性。
2017年11月到2019年7月期间,该前瞻性的2期研究招募了31名进展期mCRPC男性患者,他们既往接受过至少一次雄激素受体导向治疗。中位随访时间为18.0个月。患者干预方法为Avelumab 10 mg/kg静脉注射,每2周一次,持续24周(12个周期)。在第一次和第二次Avelumab治疗前5天,对一或两个疾病部位进行单次SABR(20 Gy)治疗。研究的主要终点是疾病控制率(DCR)。次要终点是客观反应率(ORR)、影像学无进展生存期(rPFS)、总生存期(OS)和安全性。
研究共包括31名男性患者(中位年龄71岁,71%的患者之前接受过≥2种mCRPC治疗线,81%的患者有>5个转移灶)。主要终点DCR为48%(15/31;95%置信区间[CI]30-67%),ORR为31%(5/16;95%CI 11-59%)。无放疗病灶的ORR为33%(4/12;95%CI 10-65%)。中位rPFS为8.4个月(95% CI 4.5-未达到[NR]),中位OS为14.1个月(95% CI 8.9-NR)。6名患者(16%)发生了3-4级治疗相关的不良事件,其中3名(10%)需要大剂量皮质类固醇治疗。另外,血浆雄激素受体改变与较低的DCR有关(22% vs 71%,p = 0.13)。该研究的局限性包括样本量小和没有对照组。
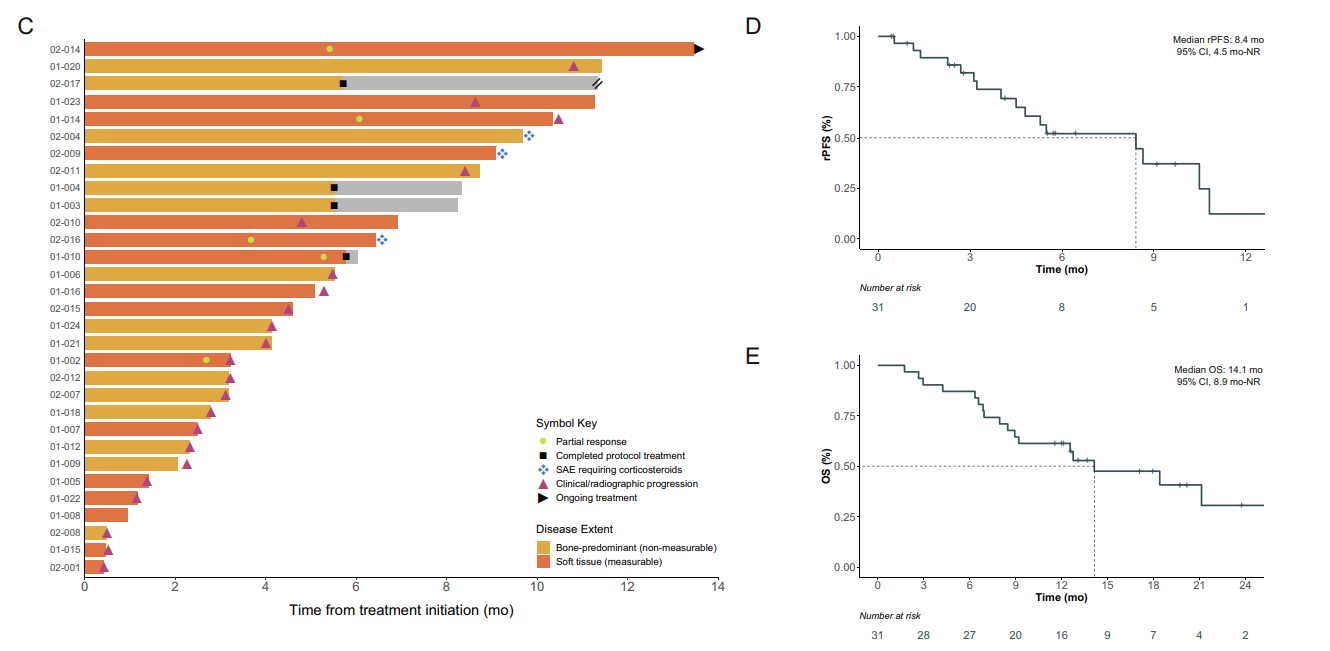
抗肿瘤活性情况
综上所述,Avelumab与SABR联用在治疗难治性mCRPC中表现出良好,且毒性可接受。该治疗组合也值得进一步的研究。
原始出处:
Edmond M Kwan , Lavinia Spain , Angelyn Anton et al. Avelumab Combined with Stereotactic Ablative Body Radiotherapy in Metastatic Castration-resistant Prostate Cancer: The Phase 2 ICE-PAC Clinical Trial. Eur Urol. Sep 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#抗性#
66
#mAb#
42
#去势抵抗性前列腺癌#
33
#avelumab#
38