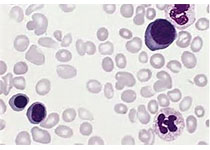
Clin cancer research:EPZ-6438联合R-CHOP治疗弥漫性大B细胞淋巴瘤
2020-07-03 QQY MedSci原创
口服EZH2抑制剂tazemetostat(EPZ-6438)可以靶向依赖EZH2活性的异常增殖,EPZ-6438联合R-CHOP是否可安全用于弥漫性大B细胞淋巴瘤?
方法:这是一项Ib期的临床试验,评估EPZ-6438联合R-CHOP用于60-80岁的新确诊的弥漫性大B细胞淋巴瘤的安全性,并明确EPZ-6438的II期试验推荐剂量(RP2D)。
结果:共招募了17位患者。在C1和C2期间,共观察到2例剂量限制性毒性:1例3级便秘(400 mg)和1例5级肺部感染(800 mg)。≥10%的患者发生的≥3级毒性作用有便秘(24%)、恶心(12%)和低钾血症(12%)。8位(47%)患者发生3-4级血液学副作用:中性粒细胞减少(47%)、白细胞减少症(29%)、贫血(18%)和血小板减少症(12%)。EPZ-6438的RP2D为800 mg。EPZ-6438剂量增加未增加对器官的毒性。800 mg剂量时,EPZ-6438的AUC和Cmax与单药研究(E7438-G000-101)的相似。
结论:EPZ-6438与R-CHOP联合的RP2D是800 mg 2/日。安全性和PK的相关性与单用R-CHOP的相当。初始疗效数据令人鼓舞,值得进行II期试验进一步验证。
原始出处:
Clémentine Sarkozy,et al. A LYSA Phase Ib Study of Tazemetostat (EPZ-6438) plus R-CHOP in Patients with Newly Diagnosed Diffuse Large B-Cell Lymphoma (DLBCL) with Poor Prognosis Features. Clinical Cancer Research. July 01, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞淋巴瘤#
36
#B细胞#
33
#弥漫性大B细胞淋巴瘤#
48
#弥漫性#
44
#R-CHOP#
48
#Research#
23