JACC:颠覆!LDL-C为残余胆固醇背了“坏胆固醇”的黑锅?
2021-01-02 MedSci原创 MedSci原创
残余胆固醇,而非LDL-C或许才是引起ASCVD的罪魁祸首?
根据既往认知,大家都已认定血液中的胆固醇和甘油三酯是血脂管理的重中之重,同时可以预测心血管事件(CVD)的发生风险。其中,高密度脂蛋白(HDL)和低密度脂蛋白(LDL)是胆固醇中的一对“死对头”——LDL将脂质带到外周组织中,HDL更多是对胆固醇的反向转运,也就是不断将胆固醇从外周组织运输到肝脏。因此,LDL-胆固醇(LDL-C)一直被认为是“坏胆固醇”。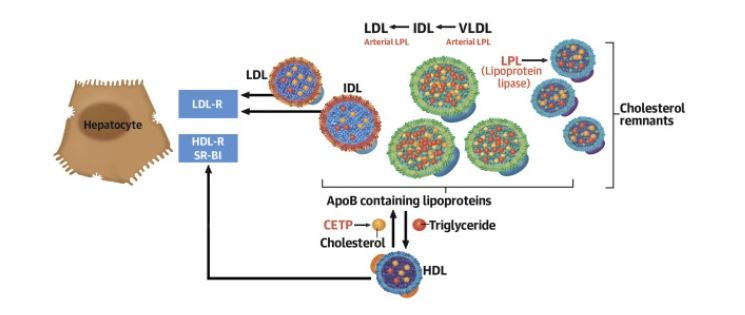
各种胆固醇的代谢通路
同时,动脉硬化是引发包括心肌梗死和动脉粥样硬化性心血管病(ASCVD)在内急性心血管事件的开端。因此,作为动脉硬化这一病变的核心驱动力——LDL-C是所有指南中一级与二级预防的主要治疗目标。
然而,最近发表在《美国心脏病学会杂志》(JACC)上的两项大型研究则激起了大家上述认知的争议:残余胆固醇,而非LDL-C或许才是引起ASCVD的罪魁祸首。残余胆固醇(Remnant-C)被定义为除了LDL-C和HDL-C外,人体内包括VLDL-C与中密度脂蛋白胆固醇(IDL-C)等两种胆固醇的含量。
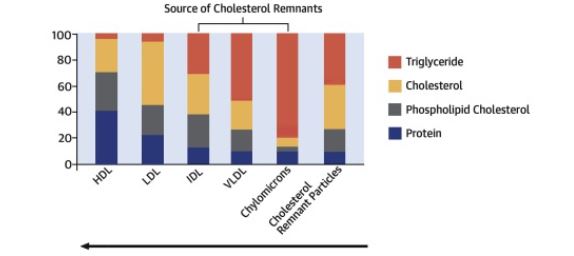
残余胆固醇的计算方式
该研究是西班牙高危一级预防PREDIMED(该研究曾在NEJM上发表论文,证明对于CVD高危人群,地中海饮食辅以特级初榨橄榄油或坚果可以降低严重CVD的发病率)的一部分。纳入的受访者7000名受访者被认为是ASCVD高危人群,被记录了血脂水平。他们的基线平均年龄为67岁,体重指数BMI为30 kg/m2。其中43%为男性;48%为糖尿病患者。在进行中位随访时间为4.8年后,评估主要CVD事件(MACEs)的发生风险。
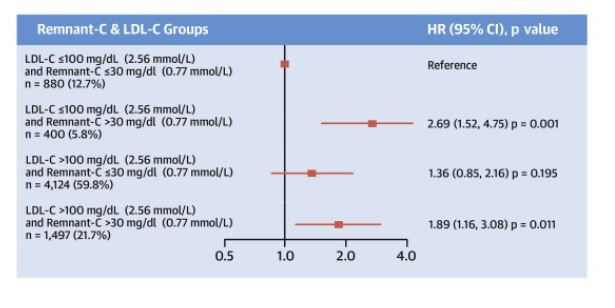
结果发现,在随访期间,3.8%的受访者出现主要不良CVD。其中,甘油三酯、非HDL-C 、残余胆固醇水平每升高10 mg/dl(分别对应0.11、0.26、0.26 mmol/L),主要CVD(包括心肌梗死、中风、心血管死亡)发生风险分别增加4%、5%、21%。但无论受访者的LDL-C还是HDL-C水平,均与MACEs的发生没有统计学相关性。
同时,当甘油三酯水平>150 mg/dl (1.69 mmol/L)且男士HDL-C水平<40 mg/dl(1.03 mmol/L)或女士HDL-C水平<50 mg/dl(1.29 mmol/L)时,主要不良CVD发生风险增加44%。
但不论LDL-C 水平为多少(≤100 mg/dl或2.59 mmol/L),残余胆固醇≥30mg/dL(0.78mmol/L)为高危界限时,主要不良CVD风险均高于参与胆固醇水平较低者。且残余胆固醇水平每升高10mg/dL,MACEs相对风险升高21%。
为此,研究者认为,如果该研究结果被进一步验证,将是对ASCVD诊断和预防的一大重要颠覆。那么未来,在进行血脂检查的时候,或许还需要将残余胆固醇甚至脂蛋白(a) 、载脂蛋白B等指标进行完善来更好评估与指导CVD预防。
参考文献:
Castañer O, et al. Remnant Cholesterol, Not LDL Cholesterol, Is Associated With Incident Cardiovascular Disease. J Am Coll Cardiol. 2020 Dec 8;76(23):2712-2724. doi: 10.1016/j.jacc.2020.10.008.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
45
#残余胆固醇#
41
#ACC#
48
#LDL#
55
已读,受益匪浅
121
新的发现将导致研究方向发生位移!
106
好文章!
108