JAMA Netw Open:乳腺癌和卵巢癌患者致癌变异的携带情况
2021-03-04 MedSci原创 MedSci原创
遗传性乳腺癌和卵巢癌综合征相关基因的有害变异是否与说英语和克里奥尔语的加勒比海人群中乳腺癌和卵巢癌的发生有关?
加勒比海地区乳腺癌和卵巢癌的发病率都很高;然而,到目前为止,很少有数据量化该地区人口中遗传性癌症的流行情况。
本研究旨在明确遗传性乳腺癌和卵巢癌综合征相关基因的有害变异是否与说英语和克里奥尔语的加勒比海人群中乳腺癌和卵巢癌的发生有关。
这项研究使用了2010年6月-2018年6月巴哈马、开曼群岛、巴巴多斯、多米尼克、牙买加、海地和特立尼达和多巴哥胚系基因检测的数据。对30个基因进行二代测序和多重连接依赖探针扩增(BRCA1和BRCA2)。在研究登记时对医疗记录进行了审查。纳入至少有一位祖父母出生在研究地点的乳腺癌和卵巢癌患者。主要研究结果:遗传性乳腺癌和卵巢癌综合征的发生率以及变异类型和谱系。
共纳入了1018名受试者,其中999名(98.1%)患有乳腺癌(平均年龄46.6[10.8]岁),21名(2.1%)患有卵巢癌(平均47.6[13.5]岁)。三个人拒绝报告他们的预后。
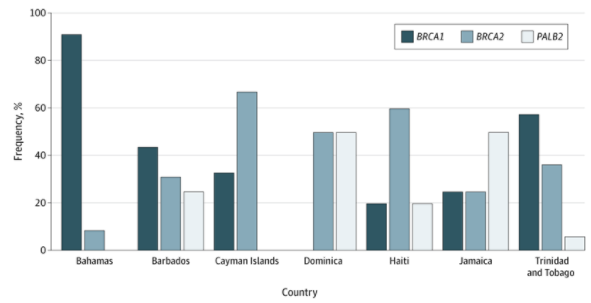
致病性/可能致病性变异在不同国家中的分布
1015名受试者中共有144名(14.2%)携带遗传性乳腺癌和卵巢癌综合征基因致病性或可能致病性(P/LP)变异。携带BRCA1、BRCA2、PALB2、RAD51C、CHEK2、ATM、STK11和NBN基因P/LP变异的患者比例分别为64%、23%、9%和4%。
有无携带变异的患者特征
变异携带者的平均年龄(SD)为40.7(9.2)岁,而非携带者为47.5(10.7)岁。巴哈马的遗传性乳腺癌和卵巢癌的比例最高(23%),其次是巴巴多斯(17.9%)、特立尼达(12%)、多米尼加(8.8%)、海地(6.7%)、开曼群岛(6.3%)和牙买加(4.9%)。
携带不同变异的患者特征
在加勒比海地区出生的患有乳腺癌的女性和男性中,有一级或二级家庭成员患有乳腺癌与任何BRCA1或BRCA2胚系变异有关(优势比 1.58;95%CI 1.24-2.01;P<0.001)。BRCA1和BRCA2变异与三阴性乳腺癌的相关性更强(优势比 6.33;95%CI 2.05-19.54;P=0.001)。
总而言之,这项研究表明,在加勒比海地区出生的乳腺癌和卵巢癌患者中,每7人中就有1人为遗传性乳腺癌/卵巢癌。遗传性乳腺癌和卵巢癌的比例因地区而异,从巴哈马的23%到牙买加的4.9%不等。每个岛屿都有其独特的突变。
原始出处:
George Sophia H L,Donenberg Talia,Alexis Cheryl et al. Gene Sequencing for Pathogenic Variants Among Adults With Breast and Ovarian Cancer in the Caribbean. JAMA Netw Open, 2021, 4: e210307.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#乳腺癌和卵巢癌#
37
#NET#
28
#PE#
36
已看,还可以。
76
#变异#
37
#致癌#
36
#癌变#
40
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
44
携带BRCA1、BRCA2、PALB2、RAD51C、CHEK2、ATM、STK11和NBN基因P/LP变异的患者比例分别为64%、23%、9%和4%。
0