Nature:贵州中医药大学彭立发现神经-免疫-心血管互作通路影响动脉粥样硬化
2022-06-04 MedSci原创 MedSci原创
4月27日,国际顶级期刊《Nature》正刊发表题为“Neuroimmune cardiovascular interfaces control atherosclerosis&rdquo
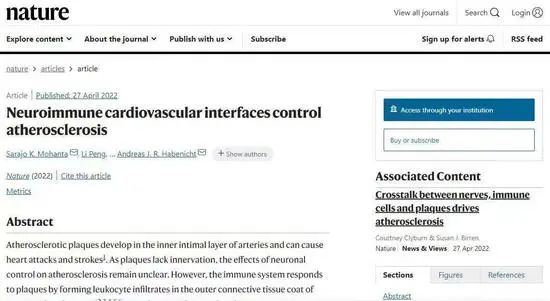
4月27日,国际顶级期刊《Nature》正刊发表题为“Neuroimmune cardiovascular interfaces control atherosclerosis”(神经-免疫-心血管互作控制动脉粥样硬化)的研究论文。贵州中医药大学第二附属医院心血管内科副教授彭立与德国慕尼黑大学Mohanta博士为共同第一作者。
该项研究中,彭立负责通过病毒示踪实验鉴定动脉-大脑-神经环路(artery-brain-circuit,ABC)所涉及的通路。研究发现,广泛分布的神经-免疫-心血管互作(neuro-immune-cardiovascular interface,NICIs)出现在小鼠和人类动脉粥样硬化中,斑块对应的外膜段显示出广泛的轴突网络,包括轴突末端的生长锥,与免疫细胞形成连接,并局限于中膜平滑肌细胞附近。
长期从事心血管疾病的基础研究的彭立表示,此次研究通过使用伪狂犬病毒跨突触示踪技术,发现了小鼠NICI建立的动脉-大脑-神经环路(artery-brain- circuit,ABC),腹主动脉外膜伤害性传入通过脊髓T6-T13背根神经节进入中枢神经系统,多个感觉和交感中枢神经系统神经元被追踪到脑干和杏仁核神经元,交感神经通过脊髓中间外侧神经元和腹腔神经节从延髓和下丘脑神经元投射到动脉外膜。
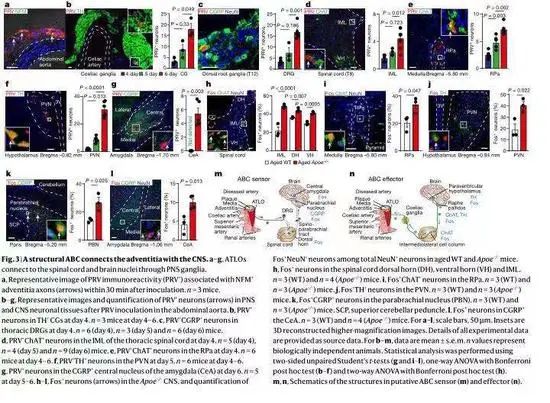
动脉外膜NICI是动脉粥样硬化的代理前哨传感器和效应器,其通过识别炎症的炎性信使来识别斑块的位置和血管发炎的位置,再将炎性信号通过神经转化为电信号传递给大脑。彭立说:“大脑处理这些信号,并将效应信号发送回发炎的血管,这会对炎症产生负面影响,导致动脉粥样硬化恶化。”
在动脉粥样硬化疾病进展期间,脾脏交感神经和腹腔迷走神经活动增加。此次研究者利用外科手术或化学药物切断了病变动脉和大脑之间的交感神经连接,8个月后比较了接受治疗的小鼠和未接受治疗的小鼠。
研究成果显示,在接受过治疗的小鼠中,动脉粥样硬化外膜神经-免疫-心血管互作解体,动脉粥样硬化病变减少,斑块稳定性增加。研究成果证明,外周神经系统利用神经-免疫-心血管互作组装动脉-大脑-神经环路,阻断该环路可减轻动脉粥样硬化。
该研究耗时12年,首次证实动脉粥样硬化斑块的血管外膜和大脑之间可以交换神经信号,从而实现大脑对动脉粥样硬化斑块的感知和控制。研究成果发布后,国际医学界给予了高度肯定,认为“神经免疫信号有助于动脉粥样硬化进展是对该领域有价值的贡献”、“这项基础研究将开创动脉粥样硬化治疗的新思路”。
同时,彭立的这一研究成果也实现了贵州中医药大学及整个贵州在《Nature》正刊发表高质量医学科研论文“零”的突破。
原始出处:
Mohanta SK, Peng L, Li Y, Lu S, Sun T, Carnevale L, Perrotta M, Ma Z, Förstera B, Stanic K, Zhang C, Zhang X, Szczepaniak P, Bianchini M, Saeed BR, Carnevale R, Hu D, Nosalski R, Pallante F, Beer M, Santovito D, Ertürk A, Mettenleiter TC, Klupp BG, Megens RTA, Steffens S, Pelisek J, Eckstein HH, Kleemann R, Habenicht L, Mallat Z, Michel JB, Bernhagen J, Dichgans M, D'Agostino G, Guzik TJ, Olofsson PS, Yin C, Weber C, Lembo G, Carnevale D, Habenicht AJR.Neuroimmune cardiovascular interfaces control atherosclerosis.Nature. 2022 May;605(7908):152-159. doi: 10.1038/s41586-022-04673-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
51
ni u n iu
23
#Nat#
29
#医药#
53
#互作#
55