J Sex Med:与精神药物有关的勃起和射精功能障碍:一项系统性回顾
2021-07-31 AlexYang MedSci原创
性功能障碍可能是使用抗精神病药物、抗抑郁药物和其他精神药物治疗的副作用。近期,有研究人员回顾了有关服用精神药物患者出现男性性功能障碍的证据,从而为非精神科医生提供管理这些功能障碍的具体信息。
性功能障碍可能是使用抗精神病药物、抗抑郁药物和其他精神药物治疗的副作用。近期,有研究人员回顾了有关服用精神药物患者出现男性性功能障碍的证据,从而为非精神科医生提供管理这些功能障碍的具体信息。

研究人员对Medline和Embase数据库进行了系统性的检索,检索的文献时间直至2020年10月15日。他们纳入了比较精神药物与安慰剂或另一种同类药物的随机对照试验,研究持续时间至少5周。
研究人员考虑了那些将男性群体与女性群体分开评估,并对男性性周期的不同阶段进行了单独分析的研究。他们在最后的审查中共纳入了41项研究。结果发现,与安慰剂相比,性功能障碍与抗抑郁药物治疗之间存在明显的关联(性欲减退OR=1.89,95%CI:1.40至2.56,22个系列,11项试验,7706名参与者;勃起功能障碍OR=2.28,95%CI:1.31至3.97,11项试验,3008名参与者;射精功能障碍OR=7.31,95%CI:4.38至12.20,19项试验,3973名参与者)。当选择性5-羟色胺再摄取抑制剂(SSRIs)与5-羟色胺/去甲肾上腺素再摄取抑制剂(SNRIs)的效果分开评估时,与安慰剂相比,只有使用SNRIs时勃起功能障碍的几率明显更高。关于抗精神病药物对男性性周期各阶段的影响,只发现了有限的数据。与其他非典型抗精神病药物相比,阿立哌唑和利培酮的勃起或射精功能障碍的几率分别较低和较高。
治疗服用精神药物患者的男性性功能障碍需要对不同的药物有基本的了解,因为这些药物以不同的机制影响性功能。研究的优势在于精神药物对勃起功能和射精的影响进行了单独评估。研究的限制在于因作用机制的巨大差异性,很难对不同类别的精神药物的作用进行比较。
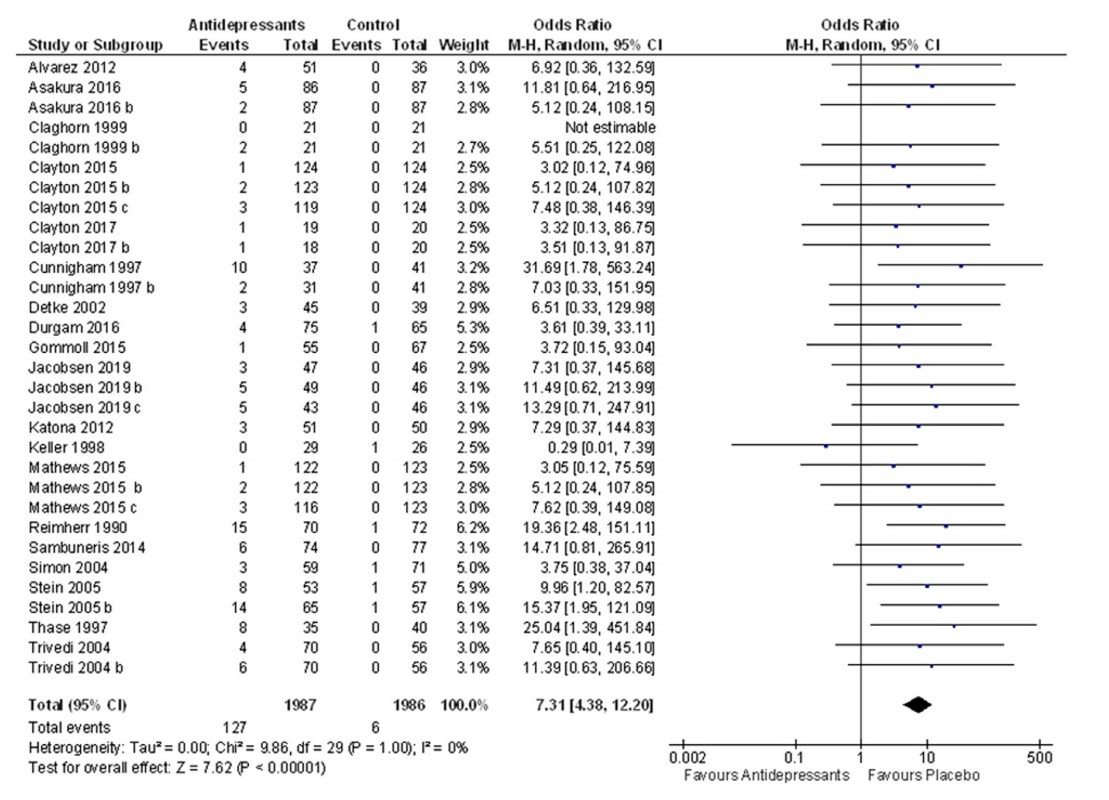
射精功能障碍与抗抑郁药物治疗相关性的随机、安慰剂对照研究
综上所述,不同的抗精神病药物对男性性功能影响的机制各不相同,大多数抗抑郁药会导致性欲减退、射精和勃起功能障碍。另外,SNRIs的使用似乎与勃起功能障碍的特定风险有关。
原始出处:
Margherita Trinchieri , Martina Trinchieri , Gianpaolo Perletti et al. Erectile and Ejaculatory Dysfunction Associated with Use of Psychotropic Drugs: A Systematic Review. J Sex Med. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#系统性#
35
#勃起#
35
#功能障碍#
46
#射精#
35
#精神药物#
41
#Med#
35