双侧双重带状疱疹
2020-07-28 刘睿 孙弦 胡珍 临床皮肤科杂志
患者女,64 岁。 因左侧头面及右侧腰腹部出现簇 集水疱伴疼痛 7 d 至我院就诊。患者 7 d 前无明显诱因 左侧头皮、额面部疼痛不适,呈间歇性刺痛,不久左侧 头皮、额部开始出现片状红斑,其上见散在
1 病历摘要
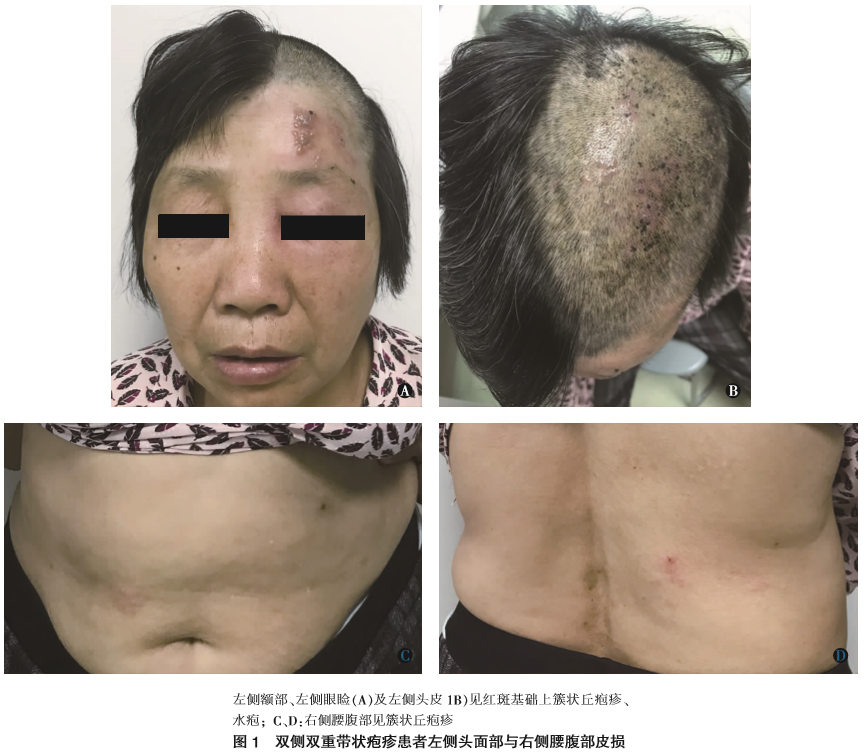
患者女,64 岁。 因左侧头面及右侧腰腹部出现簇 集水疱伴疼痛 7 d 至我院就诊。患者 7 d 前无明显诱因 左侧头皮、额面部疼痛不适,呈间歇性刺痛,不久左侧 头皮、额部开始出现片状红斑,其上见散在丘疱疹、水 疱,且右腰腹开始出现簇集丘疱疹,疼痛明显,无明显 发热等症状。未行相关治疗,皮疹逐渐增多,疼痛加重, 左侧眼睑肿胀明显,睁眼困难,视物正常。 既往身体状 况一般, 有高血压病史, 服用苯磺酸左旋氨氯地平片 (施慧达),血压控制尚可。 自诉有肾结石病史,无传染 病、肿瘤病史,无食物、药物过敏史。 体格检查:一般情况可,急性病容,无浅表淋巴结 肿大,心、肺、腹部检查未见明显异常。 皮肤科检查:左侧头皮、额部、眼睑周围见片状水肿性红斑,其上见簇 集分布的丘疱疹、水疱,少许脓疱,周围红晕明显,疱 壁薄,尼氏征(-),少许破溃、结痂,左眼睑肿胀明显 (图 1A、B);右侧腰腹部见多处簇集分布的红色丘疹、 丘疱疹,未见明显水疱、糜烂(图 1C、D)。 实验室及辅助检查:血常规示白细胞正常,单核 细胞计数 0.08×109/L [正常值 (0.1~0.6)×109/L, 以下 同], 单核细胞百分比 0.018 (0.03~0.10),C 反应蛋白 5.27 mg/L(<5 mg/L);尿常规示隐血(+),蛋白质(+); 总胆固醇 6.59 mmol/L(3.1~5.7 mmol/L),低密度脂蛋 白 4.69 mmol/L (2.2~3.1 mmol/L); 人免疫缺陷病毒 (HIV)抗体、梅毒螺旋体特异抗体均(-);心电图提示 心动过缓;腹部彩超未见明显异常。 诊断:双侧双重带状疱疹。 治疗:予以更昔洛韦钠 0.5 g 每日 1 次静脉滴注, 腺苷钴胺 1.5 mg 每日 1 次肌内注射;泼尼松 10 mg 每 日 3 次口服,共 4 d;局部康复新液湿敷、红光照射、外涂复方多粘菌素 B 乳膏等治疗。 经过 10 d 综合治疗, 皮疹全部结痂、消退,残留少许色沉、瘢痕,无明显后遗 神经痛。
2 讨 论
带状疱疹是由水痘-带状疱疹病毒 (varicellazoster virus, VZV)感染引起的一种常见皮肤病,病毒 可长期潜伏在脊髓后根神经节或颅神经节内, 在某些 诱因下被激活而发病[1]。典型带状疱疹多发生于躯体单 侧,呈带状分布的簇集水疱,伴有明显疼痛感。 有文献 证明 VZV 可潜伏于机体多个感觉神经节,而多个神经 节同时激活的情况很少见,多只局限于两个皮区,根据 其是否位于身体一侧而命名为单侧双重带状疱疹 (herpes zoster duplex unilateralis) 或双侧双重带状疱疹(herpes zoster duplex bilateralis)[2-3]。 临床上两侧同 时发病的情况比较少见,国内文献对此类患者绝大部 分以“双侧带状疱疹”命名,多侵犯对称两侧胸腰段神 经节[4-5],但本例患者同时侵犯左侧头面和右侧腰腹部, 位于不同皮区,故笔者认为“双侧双重带状疱疹”更为 准确。 双侧带状疱疹的具体发病机制目前不明确,可 能和免疫功能低下有关,多见于肿瘤患者、伴有基础 疾病的老年人、HIV 感染者、长期使用免疫抑制剂或糖 皮质激素的患者[5-6],但也有报道发生在无基础疾病的 体健患者[7-8]。 双侧双重带状疱疹治疗和常规带状疱疹 治疗基本相同,主要是及时足量的抗病毒、营养神经、 止痛等治疗。 本例患者为老年女性,有高血压史,血压 控制良好,无肿瘤病史、无免疫抑制剂服用史、HIV 抗 体阴性,但平素易劳累,睡眠欠佳,年龄偏大,考虑这些因素可能和本病发作有关。 本例患者因左侧眼睑肿 胀明显,睁眼困难,为预防继发结膜炎、虹膜炎等,予以 口服小剂量泼尼松,肿胀很快消退,未见虹膜炎、结膜 炎等并发症,未出现耳部疱疹,视力、听力正常,经过 10 d 的抗病毒和营养神经等治疗,皮疹全部消退,无后 遗神经痛,疗效良好。
参考文献
原始出处:
刘 睿,孙 弦,胡 珍,吴 庭等,双侧双重带状疱疹[J],临床皮肤科杂志,2020,49(5)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






_1583673209000.jpeg)






学习了
90
学习了
103
第一次见,学习了
102
#双侧#
33
#疱疹#
34
学习了
81