Journal of Tissue Viability:微电流疗法(EMT)能够有效促进伤口愈合
2021-12-16 小文子 MedSci原创
EMT是一种有效、安全的治疗方法,可改善伤口面积、愈合时间和疼痛。
微电流疗法(EMT)在伤口愈合过程中产生的内源性电场在细胞迁移和上皮伤口愈合中起着重要作用。Journal of Tissue Viability杂志的一项研究探讨了EMT改善急慢性伤口患者伤口愈合和疼痛的有效性和安全性。

研究人员检索相关文献,纳入截至2020年8月1日发表的评估EMT在伤口愈合有效性的随机临床试验。主要结局为伤口表面积、愈合时间和愈合的伤口数量。次要结局是疼痛感和不良事件。
纳入8项RCT研究进行定性总结,7项RCT研究进行定量分析(n = 337)。3项试验应用的波形为方形脉冲,2项研究中使用直流电。脉冲电流的频率在0.5 ~ 10Hz之间,电流强度范围为15 ~ 500 μA。3项试验采用低强度电流(≤100 μA),2项试验采用高强度电流(300 μA和500 μA),1项研究应用高强度和低强度电流(40μ- 500μ)。评价伤口愈合的主要结局为:3项研究评价了伤口表面积,4项研究评价了伤口完全愈合时间,2项研究评价了伤口愈合的数量。
EMT联合标准伤口护理(SWC)使得伤口愈合加快(MD=-8.3 cm2; 95% CI: -10.5 ~ -6.0)和愈合时间缩短(MD =-7.0 d; 95% CI:-11.9 ~ -2.1)。但是,愈合伤口的数量没有差异(RR = 2.0; 95% CI: 0.5 ~ 9.1],证据质量较低。EMT降低了感知疼痛(MD =-1.4; 95% CI: -2.7 ~ -0.2),两组间不良反应无差异(风险差异 = 0.05; 95% CI: -0.06 ~ 0.17)。
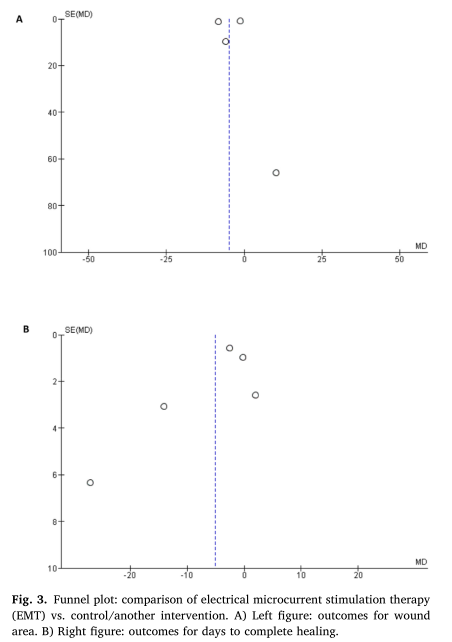
结果表明,EMT是一种有效、安全的治疗方法,可改善伤口面积、愈合时间和疼痛。临床研究应设计更加详细的干预参数和方案验证临床结局,以降低偏倚风险。
原文出处:
Juan Avendaño-Coy, Electrical microcurrent stimulation therapy for wound healing: A meta-analysis of randomized clinical trials. Journal of Tissue Viability, https://doi.org/10.1016/j.jtv.2021.12.002.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Tissue#
51
谢谢
54
学习
51
#伤口愈合#
50
#EMT#
53