JCO:基于电子化患者报告结局(ePRO)监测与自动化管理干预提醒的数字化乳腺癌病程管理(eRAPID研究)
2022-04-29 网络 网络
乳腺癌是威胁女性健康常见的恶性肿瘤之一, 也是全球女性癌症相关死亡的主要原因。尽管乳腺癌患者的5年生存率近些年有了提高,但患者在接受手术、放化疗、靶向治疗等会出现各种症状,对其生理、心理等产生诸多不良
乳腺癌是威胁女性健康常见的恶性肿瘤之一, 也是全球女性癌症相关死亡的主要原因。尽管乳腺癌患者的5年生存率近些年有了提高,但患者在接受手术、放化疗、靶向治疗等会出现各种症状,对其生理、心理等产生诸多不良影响。以往大部分乳腺癌研究是以患者的检验报告及临床结局为观察指标,忽略了对患者来说非常重要的,以患者主观感受为主的疗效评估。患者报告结局(Patient-reported outcome,PRO)是一种直接反映患者对其自身健康状况评估的报告。使用PRO捕捉患者症状,对于提供有价值、高质量以及以患者为中心的治疗至关重要。
国际顶尖肿瘤学期刊Journal of Clinical Oncology报道了英国利兹大学、圣詹姆士大学医院的Galina Velikova博士等研究人员对一个在线电子医疗系统eRAPID进行III期随机对照试验的研究结果。旨在评估在癌症化疗期间,将额外的ePRO、远程在线监测以及自动化算法驱动的患者建议引入到常规护理中,是否对患者和临床医生存在潜在益处。

(图源:Journal of Clinical Oncology)
研究方法
研究对象为开始化疗的癌症患者,大部分为乳腺癌患者,其余为妇科癌症及结直肠癌患者。他们被随机分配至常规护理组(UC)或额外增加eRAPID组(每周在线症状报告,为期18周)。试验注册: ISRCTN88520246.
常规护理:肿瘤医生根据经验对患者进行治疗管理,患者收到有关治疗相关症状的口头和书面信息。在治疗期间,肿瘤专家或诊所护士定期或通过电话评估患者的毒性并确定下一次治疗方案。报告的症状记录在急性分诊表上。化疗期间的医疗问题通过急性肿瘤学服务进行管理。患者通过紧急热线与医院联系,急性直接入医院肿瘤科。
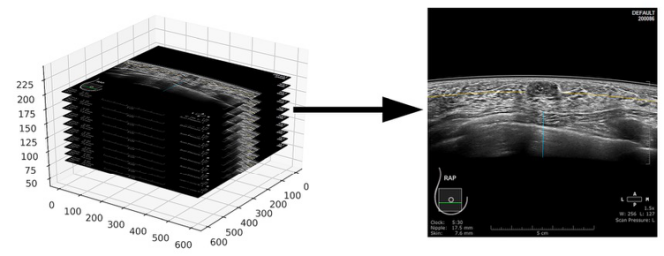
eRAPID组:在常规护理的基础上,还对患者进行基于ePAPID系统的管理。患者在家使用自己的电脑或移动设备,在18周内完成在线症状问题。每周通过短信或电子邮件发送提醒。患者会立即收到有关症状管理的严重程度依赖性建议或联系医院的提示。症状报告会在电子病历中实时显示。严重症状报告的警报信息会发送到每个临床团队共享的电子邮箱,由护士监控。
eRAPID系统将ePRO症状报告与定制临床算法相结合,为患者提供基于严重程度的自动化建议,以支持患者自我管理或联系医院。关于症状的问卷和建议由一个多学科项目团队开发,参与者包括肿瘤科临床医生、健康信息学专业人员以及患者。开发团队与多个癌症小组合作,选择并确认与治疗相关的关键症状及严重程度,并制定针对患者的建议和电子邮件提醒的临床算法。研究团队开发了五种分层算法,对应于常见不良反应事件评价标准 (CTCAE)和英国肿瘤护理学会分类表(UKONS)严重程度级别0-3,范围从A1(最严重)到D(最不严重)。患者能够通过严重程度依赖性算法问卷评分获得适当的管理建议。对于触发A1的严重症状,会自动向临床医生发送电子邮件通知,建议他们在电子病历中查看PRO报告。
主要结局:在6、12和18周评估的症状控制(癌症治疗常规功能评估,身体健康分量表FACT-PWB)。次要结果是护理流程(入院或化疗),患者自我效能和整体生活质量(癌症治疗常规功能评估、EQ5D-VAS和EORTC QLQ-C30总体评分)。采用多变量混合效应重复测量模型进行分析。
研究结果显示,参与者中,有508例患者(占690例符合纳入标准患者的73.6%)和55名卫生专业人员。与常规护理组相比,eRAPID组在第6周 (P = 0.028) 和12周(P =0 .039) 时的身体健康状况有所改善,在第18周(主要终点)时没有差异 (P = 0.69)。在第12周时,与常规护理组(56%)相比,在 12 周时,eRAPID组有更少的患者(47%)具有临床意义的身体健康恶化。
亚组分析发现非转移组在第6周明显获益(P = 0.0426),但对转移性疾病无益处。入院或化疗给药没有差异。在第18周时,使用eRAPID的患者在EQ5D-VAS量表中表现出更好的自我效能(P =0 .007)和更好的健康状况(P =0 .009)。患者对每周症状报告的平均依从率是64.7%。患者的依从性与临床医生的数据使用相关,并在12周时,与FACT-PWB的改善具有相关性。
结果显示,通过ePRO系统进行实时监测可改善主要以治愈为目的的患者群体的身体健康(6 周和 12 周)和自我效能感(18 周),而不会增加医院工作量。
研究启示
这些发现证明了远程实时监测在常规癌症治疗中是可行的,特别是在COVID-19大流行情况下;也是治疗性化疗期间的另一种数字化护理模式,可以帮助轻、中度症状的癌症患者改善身体状况,减少医院就诊次数,甚至能改善生活质量和长期生存。
将来数字化临床试验(DCT)模式随着不断探索,将越来越成熟。通过研究设计,辅助ePRO,甚至辅助一些硬件(电子药盒,POCT小型化检测设备),让DCT越来越接近现实。
原始出处:
Absolom K, Warrington L, Hudson E, Hewison J, Morris C, Holch P, Carter R, Gibson A, Holmes M, Clayton B, Rogers Z, McParland L, Conner M, Glidewell L, Woroncow B, Dawkins B, Dickinson S, Hulme C, Brown J, Velikova G. Phase III Randomized Controlled Trial of eRAPID: eHealth Intervention During Chemotherapy. J Clin Oncol. 2021 Mar 1;39(7):734-747. doi: 10.1200/JCO.20.02015. Epub 2021 Jan 8. PMID: 33417506.
Basch E, Leahy AB, Dueck AC. Benefits of Digital Symptom Monitoring With Patient-Reported Outcomes During Adjuvant Cancer Treatment. J Clin Oncol. 2021 Mar 1;39(7):701-703. doi: 10.1200/JCO.20.03375.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#管理干预#
57
#ERA#
69
#JCO#
47
#自动化#
50
#数字化#
51
#PRO#
0
#患者报告结局#
64
***,谢谢分享
67