J Altern Complement Med:针刺和有氧间歇训练均可有效改善非酒精性脂肪肝患者的肝功能,其中针刺的效果更佳
2020-12-08 MedSci原创 MedSci原创
非酒精性脂肪性肝病(NAFLD)是影响肝脏的最常见和最重要的疾病之一,在全世界的发病率越来越高。本研究旨在对比针刺(EA)与有氧间歇训练(AIT)运动的效果,以及它们对非酒精性脂肪肝患者肝功能的影响,
非酒精性脂肪性肝病(NAFLD)是影响肝脏的最常见和最重要的疾病之一,在全世界的发病率越来越高。本研究旨在对比针刺(EA)与有氧间歇训练(AIT)运动的效果,以及它们对非酒精性脂肪肝患者肝功能的影响,研究结果已在线发表于J Altern Complement Med。

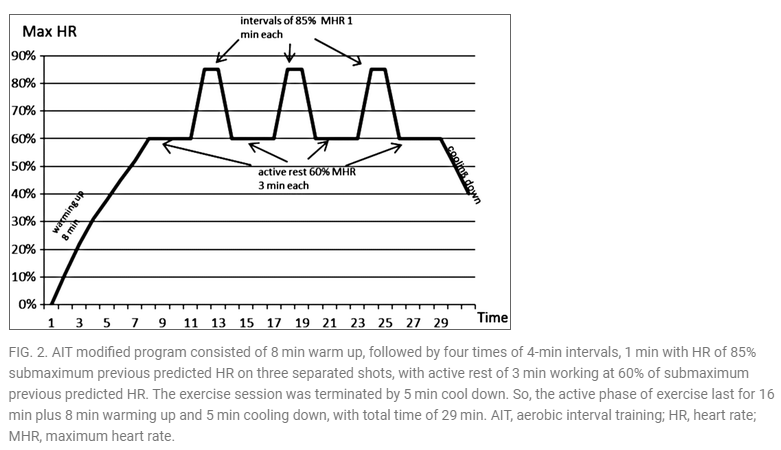
研究纳入50名年龄在30~55岁的非酒精性脂肪肝女性患者,将其随机分为两组:A组接受(EA)肝3(LR3)、肝14(LR14)、胆囊34(GB34)、胃36(ST36)等穴位的刺激,B组接受AIT锻炼。除接受标准药物治疗外,所有患者每周接受3次上述治疗,持续6周(不间断18次治疗)。治疗前后评估所有患者丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、甘油三酯(TGs)和C-反应蛋白(CRP)的水平。
结果显示,两组患者的ALT、AST、TG和CRP在经过6周的治疗后均显著下降(P<0.05)。治疗后ALT、AST和TG在两组之间均有显著差异(P<0.05),但CRP无显著差异(P>0.05)。
综上所述,该研究结果表明,EA和AIT运动都可有效改善非酒精性脂肪肝患者的肝功能,其中EA的效果更好。
原始出处:
Ramy Salama Draz, Zahra M H Serry, et al., Electroacupuncture Versus Aerobic Interval Training on Liver Functions in Patients with Nonalcoholic Fatty Liver. J Altern Complement Med. 2020 Jan;26(1):51-57. doi: 10.1089/acm.2019.0182.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#酒精性脂肪肝#
31
#ALT#
38
#Complement#
42
#Altern#
42
#MPL#
38
#酒精性#
31
#非酒精性#
31
见和最重要的疾病之一,在全世界的发病率越来越高。本研究旨在对比针刺(EA)与有氧间歇训练(AIT)运动的效果,以及它们对
73
见和最重要的疾病之一,在全世界的发病率越来越高。本研究旨在对比针刺(EA)与有氧间歇训练(AIT)运动的效果,以及它们对
71
学习了
87