JAHA:QT间期动态变化与心血管结局
2021-09-28 MedSci原创 MedSci原创
使用来自连续心电图检查的纵向信息可以提高对CVD结局的预测能力。与线性斜率或均方根误差相比,校正的长期平均QT与CVD结局的相关性更强。这一新证据具有临床意义,因为心电图经常使用、无创且价格低廉。
长QT与室性心律失常、心血管疾病(CVD)死亡率和心源性猝死相关。然而,迄今为止,还没有研究调查真实世界中不同个体QT随时间变化的动态与CVD事件和全因死亡风险之间的关系。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,这项针对北加州综合医疗保健提供系统成员的队列研究,包括61455名受试者(平均年龄为62岁;60%为女性,42%为非白人),具有3次或以上心电图检查结果(2005-2009年为基线;平均值±SD随访时间为7.6±2.6年)。
在完全调整的模型中,第3三分位数与第1三分位数相比,平均QT校正(使用Fridericia校正)与心脏骤停(风险比[HR]为1.66)、心力衰竭(HR为1.62)、室性心律失常(HR为1.56)相关、所有CVD(HR为1.31)、缺血性心脏病(HR为1.28)、总卒中(HR为1.18)和全因死亡率(HR为1.24)。
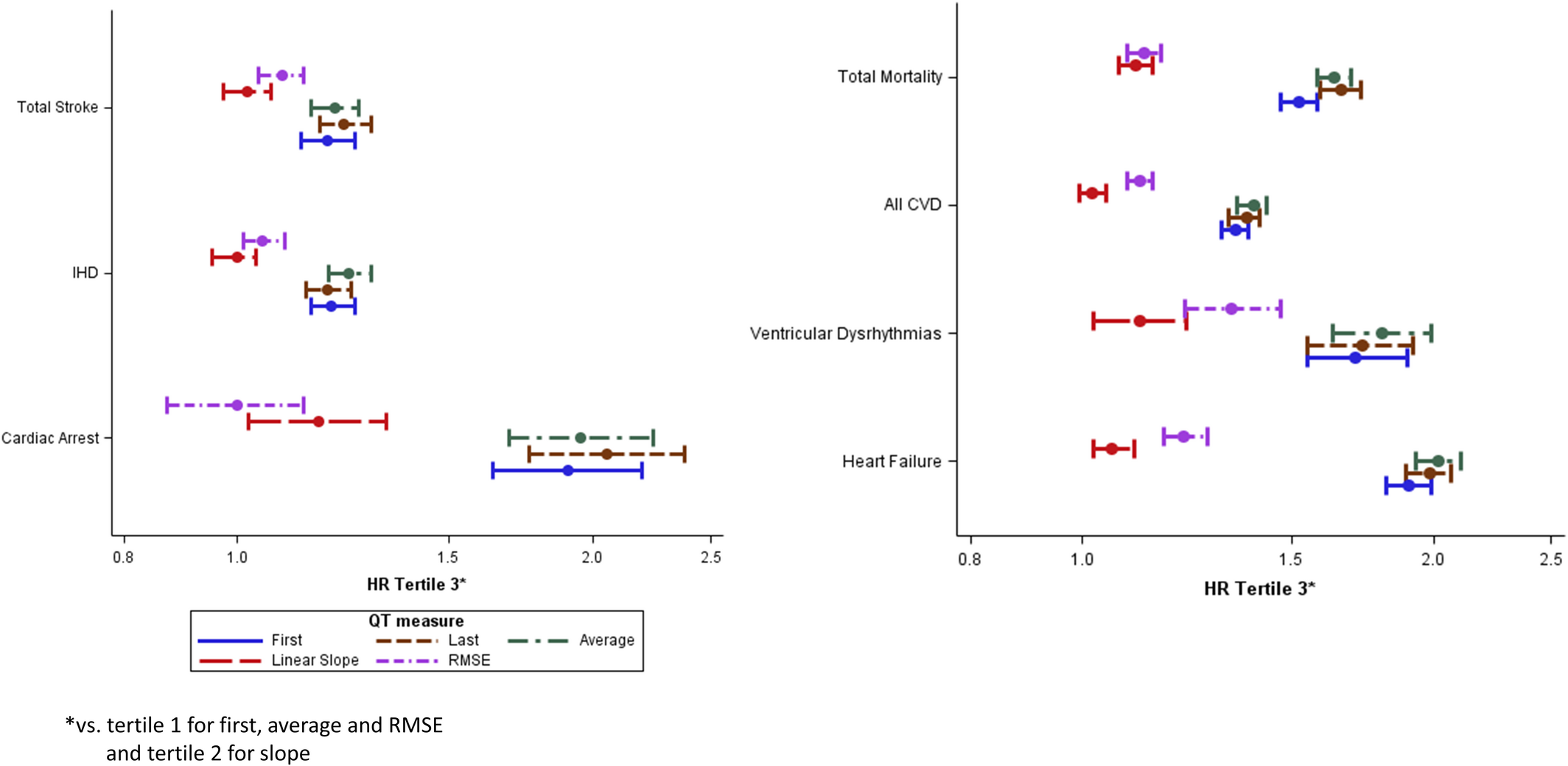
第3个三分位数与第2个三分位数相比,QT校正线性斜率与心脏骤停(HR为1.22)、室性心律失常(HR为1.12)和全因死亡率(HR为1.09)相关。第3个三分位数与第1个三分位数相比,QT校正的均方根误差与室性心律失常(HR为1.34)、心力衰竭(HR为1.28)、全因死亡率(HR为1.20)、所有CVD(HR为1.14)、总卒中(HR为1.08)和缺血性心脏病(HR为1.07)相关。
该研究的结果表明,使用来自连续心电图检查的纵向信息可以提高对CVD结局的预测能力。与线性斜率或均方根误差相比,校正的长期平均QT与CVD结局的相关性更强。这一新证据具有临床意义,因为心电图经常使用、无创且价格低廉。
原始出处:
Neha Mantri.et al.QT Interval Dynamics and Cardiovascular Outcomes: A Cohort Study in an Integrated Health Care Delivery System.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.018513
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动态变化#
44
#AHA#
46
#心血管结局#
40
#QT间期#
46