Neurology:24例LGMDR12成人患者两年随访的前瞻性自然史研究:定量MRI和临床结果评估
2022-06-30 Naomi MedSci原创
肢体-Girdle肌营养不良症常染色体隐性遗传性12型(LGMDR12)一种罕见的遗传性肌营养不良症。Biodex®等长肌力测力仪可捕捉LGMDR12患者一年中肌肉力量损失,并作为未来临床预后指标。
肢体-Girdle肌营养不良症常染色体隐性遗传性12型(LGMDR12)是一种罕见的遗传性肌营养不良症,目前缺乏改善预后措施。近日,一项发表在Neurology上的研究评估了跟踪疾病进展的定量MRI和临床结果指标,以确定哪些测试在未来的临床试验中可能有用,以评估潜在的治疗方法。
研究人员前瞻性地测量了所有参与者在基线以及1年和2年后的以下结果:6分钟步行距离(6MWD)、10米步行试验(10MWT)、医学研究委员会(MRC)总分、Biodex®等长肌力测力仪、血清肌酸激酶(CK)和大腿6点Dixon MRI。
- 研究包括24名经基因确认的成人LGMDR12患者和24名年龄和性别匹配的健康对照。
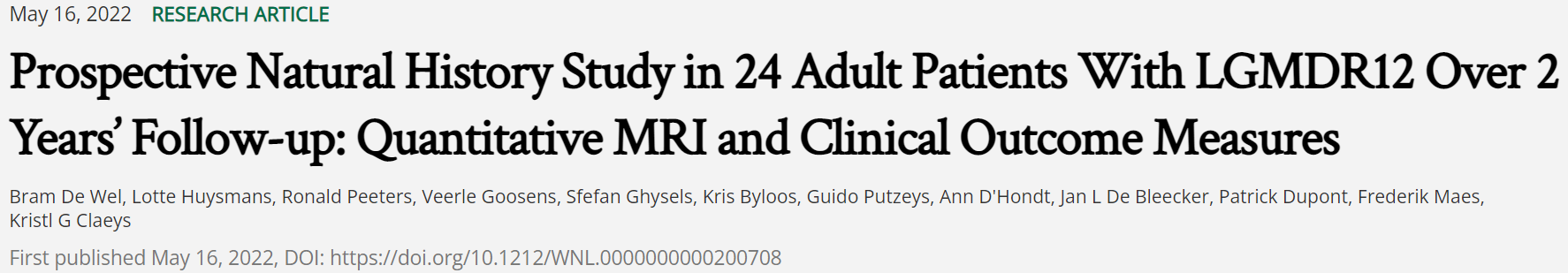
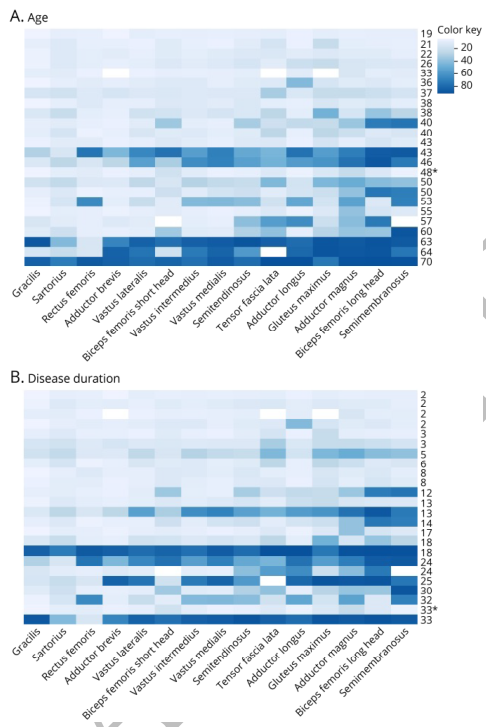
- 接受中期大腿肌肉脂肪置换的患者(质子密度脂肪分数(PDFF)为20-70%)在一年后评估的14个大腿肌肉中,有8个已经显示出PDFF显著增加。
- 标准化反应平均数(SRM)显示该组中6块肌肉在2年内对PDFF的变化有较高的反应能力。然而,在早期(<20%)或终末期(>70%)肌肉脂肪置换的患者中,PDFF在两年的随访中没有显著增加。
- Biodex®等长肌力测力仪显示,所有患者的右、左腿肌肌力(分别为-6.2 Nm,p<0.002和-4.6Nm,p<0.009)和右股四头肌(-9 Nm,p=0.044)的肌力显著下降,而6MWD、10MWT和MRCsum评分即使在两年后也没有检测到肌肉功能/力量的显著下降。在基线时,大腿全长PDFF与临床结果指标之间存在中等强度的相关性。
在选定的LGMDR12患者中,即使在一年的随访后,大腿肌肉PDFF成像也是一种跟踪进行性肌肉脂肪替代的敏感结果指标,并与临床结果指标相关。Biodex®等长肌力测力仪可以可靠地捕捉LGMDR12患者一年中肌肉力量的损失,并应作为未来临床试验的结果指标。
文献来源:De Wel B, Huysmans L, Peeters R, et al. Prospective Natural History Study in 24 Adult Patients With LGMDR12 Over 2 Years' Follow-up: Quantitative MRI and Clinical Outcome Measures [published online ahead of print, 2022 May 16]. Neurology. 2022;10.1212/WNL.0000000000200708. doi:10.1212/WNL.0000000000200708
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






















#结果评估#
36
#定量MRI#
47
#临床结果#
36
#MDR#
48
#自然史#
31
#前瞻性#
39
#Neurol#
28