IBD: 抗TNF疗法可降低炎症性肠病患者大肠癌的发生率
2020-10-21 MedSci原创 MedSci原创
炎性肠病(IBD)是一种慢性炎性疾病,包括2种主要表型:克罗恩病(CD)和溃疡性结肠炎(UC)。 IBD的发病率在全球范围内越来越高。
炎性肠病(IBD)是一种慢性炎性疾病,包括2种主要表型:克罗恩病(CD)和溃疡性结肠炎(UC)。 IBD的发病率在全球范围内越来越高;在西方国家中较高,但在新兴工业化国家中,发病率似乎增长最快。众所周知,在IBD患者中长期的肠道炎症会导致结直肠癌(CRC)的发生率高于一般人群,大肠癌似乎在IBD患者中更具侵略性,并且这些患者的死亡率要比那些没有IBD的患者更高。此外,IBD中的CRC发病年龄往往更早,并且更有可能是多灶性的。目前,尽管在IBD患者中生物制剂的使用越来越普遍,但是它们对结直肠癌发生的影响仍然不清楚。本项研究旨在通过使用大型数据库描述生物制剂对IBD患者中CRC的影响。

研究人员对1999年至2020年在美国多家医院的电子数据库中的患者进行了回顾性研究。将确定诊断为IBD的患者纳入本项研究,然后进行了多变量分析,以调整多种因素,包括药物和手术疗法,观察生物制剂对IBD患者中CRC的影响。
在1999年至2020年之间,数据库中共有62007510例患者。其中,225090(0.36%)人患有克罗恩病,而188420(0.30%)人患有溃疡性结肠炎。使用多因素分析调整混杂因素后,IBD患者更可能患CRC。在IBD人群中,接受抗TNF药物治疗的患者发生CRC的可能性较小。克罗恩病患者(OR 为0.69;95%置信区间0.66-0.73); 与溃疡性结肠炎患者(OR:为0.78;95%置信区间0.73-0.83; P<0.0001)。
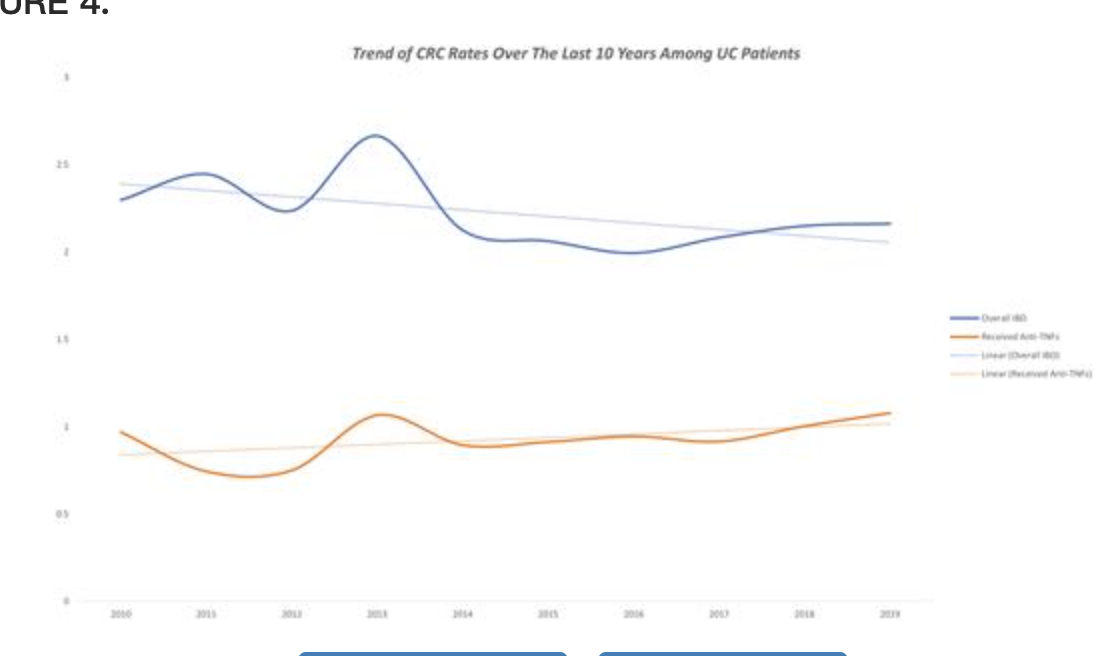
研究人员最后说道:使用抗肿瘤坏死因子药物治疗的IBD患者不太可能患CRC。这可能与生物制剂通过炎症控制和黏膜愈合在IBD患者中提供了保护作用。
原始出处:
Motasem Alkhayyat. Et al. Lower Rates of Colorectal Cancer in Patients With Inflammatory Bowel Disease Using Anti-TNF Therapy. Inflammatory Bowel Diseases.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发生率#
35
学习
73
#抗TNF#
42
#IBD#
0
#TNF#
32
#炎症性#
32
#炎症性肠病患者#
33
#IBD指南#最新研究
105