无脊髓神经损伤严重胸椎骨折脱位1例
2018-12-24 谢春生 叶小伟 王华锋 中国骨与关节损伤杂志
胸椎椎管相对狭窄,而且胸脊髓血供脆弱,一旦胸椎发生骨折脱位,约80%的患者合并完全性脊髓损伤。无脊髓神经损伤严重胸椎骨折脱位罕见,既往文献多为个案报道。笔者回顾性分析于2017-10诊治的1 例无脊髓神经损伤严重胸椎骨折脱位,并进行相关文献复习,报道如下。
胸椎椎管相对狭窄,而且胸脊髓血供脆弱,一旦胸椎发生骨折脱位,约80%的患者合并完全性脊髓损伤。无脊髓神经损伤严重胸椎骨折脱位罕见,既往文献多为个案报道。笔者回顾性分析于2017-10诊治的1 例无脊髓神经损伤严重胸椎骨折脱位,并进行相关文献复习,报道如下。
病例报道
患者,男,31 岁,因车祸伤导致胸背部剧烈疼痛、憋闷、呼吸困难1 h 余急诊入院。入院查体:患者神志清楚,精神差,胸廓挤压试验阳性,双肺呼吸音弱,胸椎中段脊柱压痛、叩击痛明显,局部明显后凸畸形,无异常感觉平面,四肢感觉、肌力及反射正常,会阴部感觉正常,肛门反射及提睾反射正常,病理征阴性。影像学检查显示多发肋骨骨折、双肺明显挫伤,双侧胸腔积血、积液,以左侧明显;T7、8椎体粉碎性骨折伴脱位。
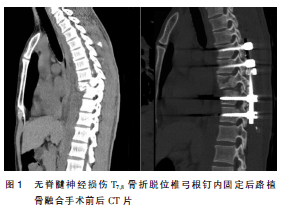
入院诊断:胸椎骨折脱位、肋骨骨折、肺挫伤并血气胸。脊髓功能AISA 分级为E 级。入院后严格卧床制动,行胸腔闭式引流,待情况稳定后行胸椎后路椎板切除减压、椎弓根钉复位固定、后外侧植骨融合术。全身麻醉后取俯卧位,作后正中切口,逐层显露,见T7、8棘突移位,T7右侧椎板、左侧椎弓根骨折,T7~10右侧横突骨折。于T6、T9、T10双侧及T7左侧置入椎弓根钉,咬除T7、8棘突,切除T7下位部分椎板及T8全椎板进行充分减压,直视下见硬膜囊完整,无明显挫伤,硬膜囊搏动好。双侧分别安装预弯连接棒(硬棒,预弯角度略小于生理曲度),间断、交替适度撑开,透视明确骨折椎体复位良好后,锁紧螺钉固定连接棒,安装横连杆。冲洗切口,于T6~10关节突关节去骨皮质至粗糙,修剪减压的自体骨粒行关节突关节植骨融合,留置引流管负压引流,逐层缝合切口。术后患者无肌力、皮肤感觉、反射等异常,复查CT 三维重建显示骨折脱位获得良好复位及矫正,内固定位置良好。术后第3 天支具保护下离床活动。术后3 个月复查CT 及X线片显示内固定位置良好,脊柱序列维持良好,骨折处获得骨性愈合,后方植骨融合良好(图1)。
讨论
胸椎的稳定性相对较好,因此胸椎(尤其是中上胸椎)骨折脱位多为高能量损伤导致,最常见于车祸伤及高处坠落伤,创伤大且受伤机制较为复杂。胸椎椎管相对狭窄,胸脊髓缓冲间隙小,并且胸脊髓的血供相对较少,胸椎骨折脱位常合并严重脊髓神经损伤。有文献报道胸椎骨折脱位患者截瘫的发生率高达80%,而无明显脊髓神经损伤者较为罕见,发生率仅为3%。由于不合并脊髓神经损伤胸椎严重骨折脱位的患者较为罕见,而且其发生机制及治疗措施有其特殊性。胸椎骨折脱位患者多合并严重多发伤,应首先处理危及患者生命的损伤,全身情况稳定后再尽早处理骨折脱位,但骨折脱位延迟处理可能会导致骨折脱位难以复位。由于此类患者无明显神经损伤症状、体征,而普通X 线片又不能很清楚显示该部位脊髓损伤情况,因此有很大一部分患者被漏诊或误诊,因此建议及时行胸椎CT 三维重建及MRI 检查以明确诊断,避免漏诊或延误诊断。胸椎骨折脱位而未造成脊髓神经损伤的可能机制为旋转、剪切应力集中于椎弓根处,从而导致椎弓根骨折,使得椎体与后方结构分离,造成椎管的容积相应扩大,暴力绕过脊髓传递至椎管前方,使脊髓未受损。本例T7左侧椎弓根断裂、椎弓根与椎体分离、椎管完整性破坏、骨性椎管扩大,而MRI 未见脊髓明显受压及信号改变。
无脊髓神经损伤严重胸椎骨折脱位的治疗,各家报道不一。通过文献复习笔者发现,早期由于手术技术的局限性,有很大一部分患者采取非手术治疗。非手术治疗措施主要为Halo 股骨牵引或严格卧床制动,由于严重影响生活质量,加上长期卧床导致各种并发症发生,目前临床已不采用。早期脊柱内固定技术的局限性使得单纯依靠后路内固定很难满意地重建脊柱正常序列,而单纯前路的结构性支撑又常常不够稳定,因此早期患者的手术方式通常为后路原位植骨融合或前后路联合手术。Shapiro 等通过复习文献发现,纳入11 例无脊髓神经损伤的胸椎骨折脱位,5 例采取非手术治疗,4 例采取后路原位植骨融合手术,单纯前路和前后路联合手术各1 例,尽管均获得骨性愈合,但仅1 例轻微骨折脱位较好地恢复了脊柱正常系列,其余均为原位畸形愈合。
随着手术技术和脊柱内固定系统的发展,胸椎骨折脱位的手术方式集中于单纯前路手术和单纯后路手术。Tong 等认为胸椎骨折脱位累及脊柱三柱结构,单纯行后路手术存在脱位椎体复位差、内固定失效、骨折不愈合等风险,而且单纯后路对于前中柱的重建存在一定困难,因此其建议行单纯前路减压、复位、支撑植骨融合;其报道3 例单纯前路手术治疗不合并脊髓神经损伤的严重胸椎骨折脱位,均获得了良好的临床疗效,恢复了脊柱正常序列。但前路手术也存在手术操作复杂、并发症多等缺点,而且此类患者由于常常合并胸腔重要脏器损伤,这大大增加了前路手术的风险。胸椎的稳定性除了由脊柱三柱结构提供外,肋骨和胸骨的环状结构也有助于增强胸椎的稳定性及应力的传递和分散,加上胸椎椎弓根钉的广泛应用,因此多数学者认为单纯后路减压、椎弓根钉复位固定、植骨融合术可以达到理想治疗效果。本例采取单纯后路手术,术中置钉后先行椎板切除减压,用预弯角度略小于生理曲度的硬棒直视下复位,复位满意后行关节突关节植骨融合,获得满意疗效。
原始出处:
谢春生;叶小伟;王华锋;等;无脊髓神经损伤严重胸椎骨折脱位1例报道并文献复习;《中国骨与关节损伤杂志》2018年第11期
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#损伤#
33
#胸椎#
40
#脱位#
31
#神经损伤#
37