患者信息
患者女性,18岁。
主诉:进食后腹胀4年,发现胰腺肿物2个月。
现病史:患者4年前出现进食后腹胀,减少进食量可缓解。于2016年8月1日晨无明显诱因出现左上腹针刺样疼痛,无放射、转移,蜷缩时缓解,无明显加重因素,持续2天后缓解,伴恶心、呕吐,呕吐物为胃内容物及胆汁,无发热、腹泻、黄疸、呕血、黑便、停止排便排气等不适。
血常规:WBC 8.73×109/L,NEUT% 76%,HGB 128g/L,PLT 235×109/L;
胰功:AMS 63U/L,LIP 18U/L;
血CEA、CA19-9、CA724、CA242未见异常
既往史:无特殊
影像检查

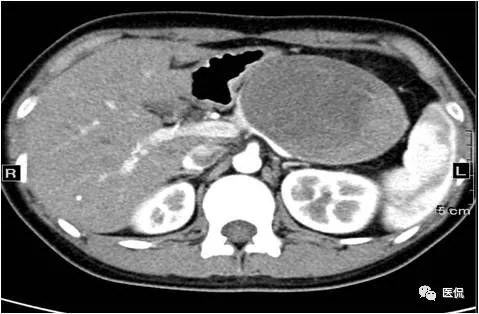
CT轴位平扫
CT增强动脉期

CT增强门脉期

CT增强延迟期

CT增强冠状位重建
你看出这是什么病了吗?
怎么读片?
胰体尾部,囊实性肿物,囊性区主要位于中央部,实性区主要位于边缘部,呈不规则片状、结节样,增强实性成分呈渐进性明显强化,囊性成分未见明确强化,边界清楚,肿物与胰腺呈“鸟嘴征表现”,向前推压胃体,脾静脉根部受压狭窄,无侵犯、破坏。
胰腺实性假乳头状瘤
病例讨论
CT图像显示肿物与胰腺关系密切,且患者为青春期女性,肿瘤标记物未见明确异常,胰功正常,因此考虑为胰腺来源的良性或低度恶性肿瘤,主要包括:胰腺实性假乳头状瘤、胰腺导管内乳头状黏液性肿瘤、胰腺黏液性囊性肿瘤、 胰腺神经内分泌肿瘤。
鉴别诊断
胰腺实性假乳头状瘤:好发于青春期少女或年轻女性,20~25y,属于交界性或低度恶性肿瘤,CT影像学表现:外生性生长,囊实性混杂密度多见,圆形或卵圆形、分叶状,可有包膜,边界清晰,可见钙化,增强扫描实性成分渐进性中等或明显强化,略低于周围正常胰腺,包膜较明显强化 。
胰腺黏液性囊性肿瘤 :起源于胰腺导管高柱状上皮细胞,占胰腺外分泌肿瘤2%~5%,中青年女性多见(90%~95%),胰体尾部多见。分型包括粘液性囊腺瘤、交界性恶性粘液性囊腺瘤、粘液性囊腺癌,CT影像学表现:单房或多房囊性肿物,边界清楚。良性:囊壁及分隔较薄;交界恶性或恶性:较厚,不规则或有壁结节;10%CT可见钙化,增强囊壁及分隔延迟轻度强化。
胰腺导管内乳头状粘液性肿瘤:罕见,属于胰腺外分泌肿瘤,起源于胰腺导管,胰头、钩突部多见,老年男性多见,65y,多有反复发作急性胰腺炎病史,属于癌前病变,恶变率30%~35%,预后较好。
胰腺神经内分泌肿瘤:主要以功能性者胰岛素瘤为主,肿瘤较小,动脉期均匀明显强化,高于正常胰腺,门脉期一般仍高于周围胰腺实质,部分呈等密度。无功能性者一般肿瘤体积较大,常伴坏死、囊变,增强扫描主要表现为富血供特点。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#胰腺肿瘤#
41
值得借鉴与分享的经验总结,非常实用的学习资料,学习了,获益匪浅,涨知识,感谢分享!
70
#腹胀#
43