患儿9个月,男性,广东东莞人,因气促1个月,咳嗽3天,加重伴发绀4小时于3月5日12时入院。
患儿于1个月前无诱因出现气促,初时气促见于吃完奶时,伴出汗多,休息后好转,家长未予重视。以后在吃奶时也有气促,中间需停歇3-4次(每次5分钟左右)オ吃饱,吃完奶后见满头大汗,间有哭闹,哭闹时气促更明显,但无发绀。多次在当地卫生院治疗仍无改善(具体不详)。3天前受凉后流涕,发热,体温38℃,无寒战、抽搐,有咳嗽,初时干咳,后转为数声咳,有痰声但无痰咳出,气促加重。4小时前哭闹,咳剧,气促明显,伴面色发绀,拒奶。当地医院用PG等药物治疗无好转,体检发现心脏杂音,为进一步诊治来我院
病后吃奶量减少,烦躁,睡眠时易惊醒,近1天哭声低,尿量比平时少1/3,无呕吐、水肿,大便正常,无异物吸入史。既往除3次感冒(服中药好转)外,无发绀、抽搐等病史。
个人史:足月顺产,出生体重3公斤,一直母乳喂养,偶服鱼肝油及钙片。3个月会抬头,8个月出牙及独坐。已做卡介苗、百白破疫苗预防接种,服过小儿麻痹糖丸。母35岁父39岁,母孕2个月时曾发热3天,服中药后痊愈。父母非近亲婚配,均无特殊病史。
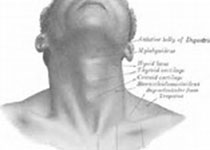
体检:T37℃,P170次/分,R68次/分,BP17/7kPa,Wt8kg。发育营养中等,反应一般,哭声低,呼吸浅促,唇及口周轻发绀,余皮肤、粘膜无发绀,无皮疹、出血点、黄染。浅表淋巴结不大,头颅五官无畸形,前囟平软,1×1cm2。巩膜无黄染,瞳孔等大等圆,对光反射存在。乳牙2只,咽充血(+)。颈软,颈静脉充盈,气管居中,甲状腺不大。胸廓无畸形,呼吸运动对称,三凹征(+)。双肺呼吸音粗,可闻及密集中小水泡音。心前区稍隆起,心尖搏动弥散,范围3x3c㎡,无震颤,心界左右扩大,心率170次/分,心律整齐,第一心音稍低,肺动脉瓣区第二心音亢进,有第三心音,于胸骨左缘第3、4肋间可闻全收缩期反流性杂音3°/6°,传导广泛,无心包磨擦音。腹平软,无包块,肝右肋下3cm,质中,边缘钝,肝颈征(+),脾左肋下未及,移动性浊音(-)。脊柱四肢无畸形,下肢无水肿,正常男童外阴,双膝反射存在,未引出病理性神经反射。
实验室检查:血红蛋白120g/L,红细胞4.0×1012/L,白细胞12.0x109/L。分类:中性0.60,淋巴0.40,血小板160×109/L。尿、大便常规正常。肝功能正常。胸片、心电图、彩色超声心动图检查已做,结果未回。
讨论
实习医生A:本例的病情特点:①9个月婴儿;②吃奶时气促1个月,3天前咳嗽、发热,气促加重,4小时前发绀;③母孕2个月时发热3天;④体征:呼吸浅促,哭声低,唇及口周轻发绀,颈静脉充盈,三凹征(+),双肺有密集中小水泡音;心尖搏动弥散,无震颤,心界扩大,心率170次/分,第一心音稍低,第二心音亢进,有第三心音,胸骨左缘第3、4肋间有全收缩期反流性杂音3级,传导广泛;肝肋下3cm,边缘钝,肝颈征(+);⑤血白细胞增高,分类中性增多;肝功正常。根据这些特点,可考虑诊断为:①支气管肺炎合并心力衰竭;②先天性心脏病?
教师:同学对支气管肺炎的掌握不错,但对心脏方面的问题似乎不够清楚或带有疑问。的确,对有心脏杂音的病例,应该排除无害性杂音。一部分婴幼儿可有心脏杂音,但杂音局限、柔和、易变化,多在2°/6°以下,无症状,不影响生长发育,更没有心脏增大,临床称之为无害性杂音。本例的特点已可排除无害性杂音,应是器质性杂音。小于3岁的器质性杂音多为先天性心脏病。本例为9个月婴儿,不单有器质性杂音,而且有气促症状,可诊断为先天性心脏病(简称先心病)。先心病有许多种类,本例属于哪一病种呢?
实习医生B:患儿主要症状为气促,气促前无发绀,气促时也无发绀,近3天合并肺炎、心衰后才出现发绀,首先考虑为左向右分流型也就是潜伏青紫型先心病。目前辅助检查结果未回,等结果回来再进一步诊断。我们已做但未有结果的检查包括胸片、心电图、彩色多普勒超声心动图。
教师:这些辅助检查是需要的,对诊断有重要作用。但我们并非等全部辅助检查结果出来后才下诊断,应该学会临床分析。小儿先心病的心脏听诊是非常重要的,部分病儿可依靠心脏杂音特征做出准确的诊断。根据本例特点,能否进一步诊断呢?
实习医生C:应该可以。左向右分流先心病常见的有室间隔缺损、房间隔缺损及动脉导管未闭,临床症状相似。房间隔缺损的杂音是胸骨左缘第2、3肋间的2到3级收缩期喷射性杂音,传导范围小,肺动脉瓣区第二心音有固定分裂。动脉导管未闭则在胸骨左缘第2肋间有连续性机器样杂音,向颈部传导。本例无连续性杂音及第二心音固定分裂,杂音最响部位又偏低在第3、4肋间,且传导广泛。不支持房间隔缺损及动脉导管未闭,可诊断为室间隔缺损。
实习医生D:不支持动脉导管未闭的还有脉压不大,无大动脉枪击音。诊断仍考虑为室间隔缺损,但为何无震颤?
教师:分析得不错,我同意大家的诊断。房间隔缺损的杂音是由于左房的血通过缺损流入右房再到右室,使右心室排血量增多,引起右室流出道相对狭窄引起的,呈喷射性。动脉导管未闭、室间隔缺损的杂音产生则是血液流经缺损部产生。动脉导管未闭时,不论收缩期或舒张期,血液均由主动脉流向肺动脉,产生连续性杂音。但如肺循环压力高时,可能只会听到收缩期杂音,而不呈连续性。所以除杂音性质外,杂音最响部位也是鉴别方法之一,合并肺动脉高压时更是重要。本例因肺动脉瓣第二音亢进,应该加上可能合并肺动脉高压的诊断。心杂音强弱与病情轻重不一定平衡。杂音响亮病情并非就重,相反,杂音轻或无杂音病情反而可能严重。室间隔缺损杂音与缺损大小、肺血管阻力有关。本例有肺炎、心衰、肺动脉高压,都可影响杂音强度。震颤除与婴儿胸壁皮下脂肪等因素有关外,与杂音强度密切相关。本例婴儿皮下脂肪厚,收缩期杂音3级,可无震颤。
实习医生E:老师,如果超声心动图检查无异常怎么办?
教师:出现这种情况机会较少,超声心动图在先心病检査诊断中起最重要的作用,但也并非100%准确。阴性结果也不能排除先心病,应结合临床及其他检查综合考虑,必要时重做。
实习医生F:老师,彩色超声心动图结果出来了。
教师:谢谢!结果显示左右心室肥大,室间隔缺损1cm,肺动脉高压(中度)。与我们刚才的分析是相符合的。
室间隔缺损是最常见的先心病,其临床表现决定于缺损的大小。小型缺损(小于0.5cm)一般无症状,仅有胸骨左缘第3、4肋间响亮粗糙的全收缩期杂音。中型、大型缺损患儿多有乏力、气促、多汗、消瘦、易发生肺炎及心衰,心界增大,心尖搏动弥漫,胸骨左缘第3、4肋间有3、4级全收缩期杂音,传导广,肺动脉瓣第二心音亢进。肺动脉高压严重时,左向右分流减少甚至出现右向左分流,心杂音减轻,患儿出现青紫。临床上特别重视肺动脉高压情况,若肺动脉高压显着,产生持续性右向左分流,可能为梗阻性肺高压,即Eisenmengre Syndrome,此时已失去手术机会。本例缺损介于中型与大型缺损之间,目前合并有支气管肺炎、心衰、肺动脉高压(中度),应如何处理?
实习医生A:我们已用二联抗生素治疗,并且用强心药西地兰,计划继续抗炎及对症处理?
实习医生G:外科手术修补缺损。
教师:强心及抗感染都是重要的,二者关系相互影响。室间隔缺损病儿肺部充血,合并心衰时肺部淤血,肺充血淤血基础上易发生肺炎。肺部体征为心衰与肺炎所合有。心衰未控制时肺部淤血,单纯用抗生素效果往往不佳。心衰治疗除强心药外,还应选用利尿剂、扩血管药。值得注意的是,与其他心衰治疗不同,应坚持规则、维持用药,防止反复发展为顽固性心衰,也为手术做好准备。
实习医生H:老师,如何掌握手术时机?
教师:单纯室间隔缺损患儿,缺损小者不一定需手术治疗,但应定期复查。中型缺损有症状者,宜于学龄前期做缺损修补术。大型缺损有内科难以控制的心衰,包括反复肺炎和生长迟缓,应及时予手术治疗。6个月至2岁婴幼儿,虽然心衰能控制,但肺动脉压持续升高、大于体循环动脉压的1/2者,亦应及早手术修补缺损。当然,具体病例应具体分析。结合本例,第一次心衰如能控制,肺动脉高压缓解,可不必手术,但需继续使用强心药并定期随访,防止心衰及肺高压再次发生、加重,至学龄前期才考虑手术治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习
86
#诊断与治疗#
29
#先天性#
0
学习啦
109
学习
88
好的
0
学习
94
学习
54
学习
30