先天性主动脉闭锁超声表现1例
2019-11-15 彭良琴 彭格红 临床超声医学杂志
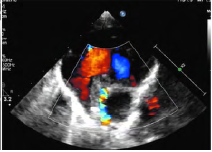
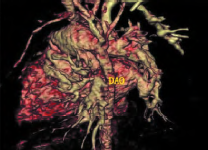
患儿女,3个月,因饮食欠佳,哭声低,生长发育差就诊。体格检查:体质量3.25kg,口唇及四肢无明显发绀,胸骨左缘可闻及3/6级收缩期杂音。超声心动图检查:心房正位,心室右襻,心脏增大,右室壁增厚,房间隔卵圆孔处回声中断约2mm,室间隔膜周部回声中断约17mm,左右肺动脉增宽与右室相连,未见主动脉与左室相连通,未见明显主动脉瓣回声(图1),主动脉根部约3mm,升主动脉约5mm,左、右冠状动脉似从主动

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#超声表现#
30
#先天性#
28
#主动脉#
38
非常精彩,受益非浅
43
非常精彩,受益非浅
71