EU:177Lu-PSMA-617 放射配体治疗高负荷转移性激素敏感性前列腺癌的新方案
2021-08-28 泌尿小王 MedSci原创
Lu-177-PSMA-617 已经在转移性去势抵抗前列腺癌(mCRPC)中进行了广泛的研究,并显示了良好的预后。该种治疗方案在一位高负荷转移性激素敏感性PCa患者中也取得了不错疗效。
大背景
前列腺癌(Prostate Cancer, PCa)患者中前列腺特异性膜抗原(prostate specific membrane antigen,PSMA)可能高于常人100至1000倍,晚期PCa患者的PSMA值可能更高。
在现有的治疗方案中,PSMA-617是目前比较理想的PSMA核素靶向药物,而Lu(镥)生物稳定性好,半衰期为6.8d,能发射β射线,可以用于肿瘤治疗,射程仅为2 mm,对骨髓功能抑制轻。镥- 177 -前列腺特定膜抗原- 617(Lutetium-177–prostate-specific membrane antigen–617,Lu-177-PSMA-617)已经在转移性去势抵抗前列腺癌(mCRPC)中进行了广泛的研究,并显示了良好的预后。该种治疗方案是否适合高负荷转移性激素敏感性PCa患者仍然缺乏研究。
最近,欧洲泌尿外科杂志发表了一例个案报道,阐述了该治疗方案在高负荷转移性激素敏感性PCa患者中的应用效果。
患者基本情况
68岁男性,新诊断为转移性激素敏感前列腺癌(mHSPC)患者,Gleason评分:3+4分;背部疼痛剧烈,ECOG评分:2分。
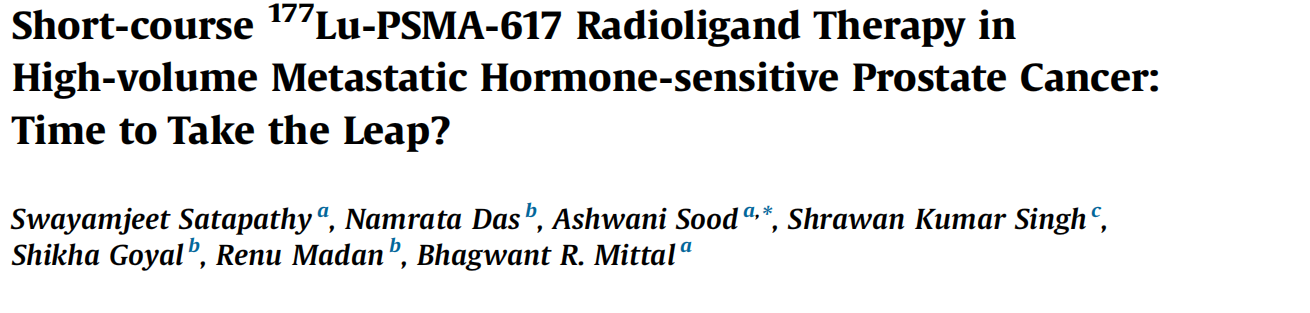
图1 68Ga-PSMA-11正电子发射断层扫描(PET)/计算机断层扫描(CT)显示前列腺示踪性病变和广泛的骨骼病变。
治疗效果
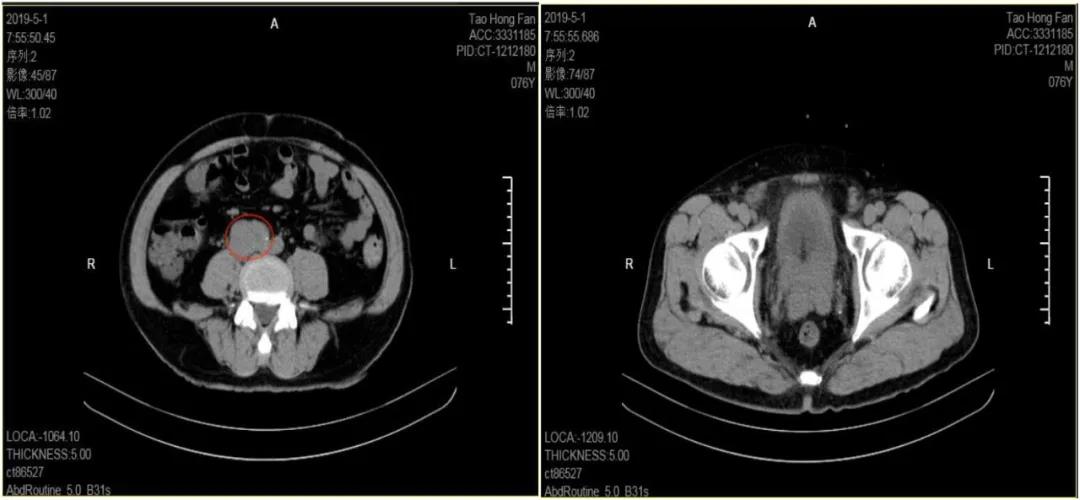
图A为治疗前的情况,作者为患者给予亮丙瑞林的雄激素剥夺治疗(ADT),并同时给予2个周期的177Lu-PSMA-617 (6.0 GBq/周期)。
患者的症状改善,在接受第一个周期治疗6周后疼痛完全缓解,他的ECOG表评分降低为0。在第二个周期后的12周,他的血清PSA从100 ng/ml下降到0.25 ng/ml(从基线下降了99.8%),重复68Ga-PSMA-11 PET/CT显示病变的范围和示踪剂的活性显著降低(图B)。
治疗期间未表现3/4级中毒症状。3个月后,他的血清PSA进一步下降到检测不到的水平(<0.2 ng/ml),并在维持ADT治疗后保持稳定。从治疗开始到第18个月,生化和放射学进展被记录下来(图1 C)患者之后开始服用恩杂鲁胺维持。
他们的研究提示了Lu-177-PSMA-617 在高容量mHSPC中的潜在应用价值。
小编认为这个个案报道显示此种治疗方案的有效性,能够为临床带来一定的启示,未来的研究中这种治疗方案可能为转移性前列腺癌的治疗带来新的方向。
参考文献
Satapathy S, Das N, Sood A, Singh SK, Goyal S, Madan R, Mittal BR. Short-course 177Lu-PSMA-617 Radioligand Therapy in High-volume Metastatic Hormone-sensitive Prostate Cancer: Time to Take the Leap? Eur Urol. 2021 Sep;80(3):390-392
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#性激素#
47
#转移性#
31
#敏感性#
46
#SMA#
36
前列腺癌相关研究,学习了,谢谢梅斯
63