肺癌筛查试验始于20世纪70年代,基于胸部X射线和痰液分析。然而,没有证据表明有任何死亡率优势。第一个低剂量计算机断层扫描(LDCT)筛查是在日本进行的,后来在1999年早期肺癌行动项目(ELCAP)的一篇里程碑式的论文中发表了利用LDCT筛查的潜力。
随后两项大型的LDCT筛查试验提供了证据,证明在LDCT筛查组招募的个体中,肺癌死亡率在统计学上有明显的下降。其中NLST试验报告了总体死亡率有小幅但明显的下降。目前欧洲已经进行了六项LDCT筛查试验,这些试验已经公布了欧洲、加拿大、日本和韩国的死亡率数据。
NLST报告显示,通过每年三次的低剂量CT(LDCT)筛查,肺癌死亡率明显降低了20%。随后荷兰-比利时的NELSON试验表明有类似的降低。近日,在国际肺癌研究协会(IASLC)举办的世界肺癌大会(WCLC)期间,英国肺癌筛查试验(UKLS)结果发表,为明确支持高危人群肺癌筛查带来了又一项重要证据,研究结果同时发表在Lancet子刊The Lancet Regional Health – Europe杂志上。
从2011年10月到2013年2月,研究人员随机分配了4055名参与者接受一次LDCT筛查邀请或不接受筛查(常规护理)。符合条件的参与者(50-75岁)在五年内患肺癌的风险评分(LLPv2)≥4.5%。通过与国家登记处的联系,收集截至2019年12月31日的肺癌病例和截至2020年2月29日的死亡数据。主要结果是肺癌导致的死亡。
结果干预组的1987名参与者和常规护理组的1981名参与者被随访了7.3年(IQR 7.1-7.6)。其中,LDCT组诊断出86例癌症,对照组为75例。筛查组有30例肺癌死亡报告,对照组有46例,筛查组因肺癌死亡风险降低近1/3(RR=0.65;95% CI 0.41-1.02)。进一步进行荟萃分析表明,9项符合条件的试验中,LDCT筛查后肺癌死亡率显著降低,总体相对率为0.84(95% CI 0.76-0.92)。
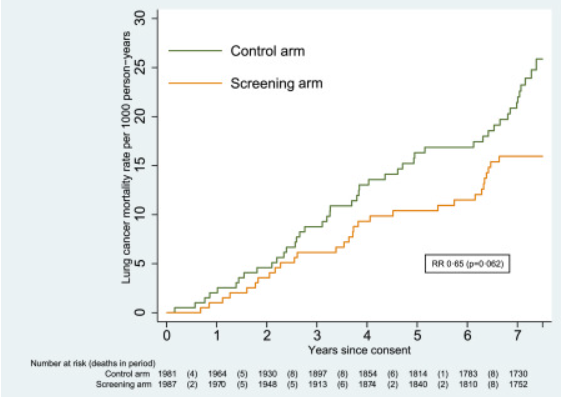
肺癌的累积死亡率。
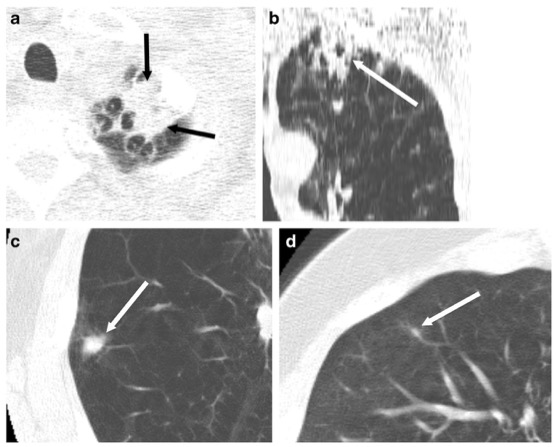
同时,筛查组中,肺癌风险随着结节数量增加而显著升高。发现3个结节的患者,后续肺癌发生风险是1个结节患者组的6倍多,而4个结节的患者,风险更是1个结节患者组的12倍多。
UKLS单次LDCT试验表明,单次胸部CT筛查,就能降低1/3肺癌死亡率!该研究为确定的风险群体的肺癌筛查提供了明确的支持。
参考文献:
Lung cancer mortality reduction by LDCT screening: UKLS randomised trial results and international meta-analysis. https://doi.org/10.1016/j.lanepe.2021.100179
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Lancet#
30
#肺癌死亡率#
36
#CT筛查#
39
#胸部CT#
46
#WCLC#
44
学习学习
48