特发性肺纤维化(IPF)患者肺康复的依从性和临床疗效,尤其是与慢性阻塞性肺病(COPD)患者相比,仍然不确定。发表在CHEST杂志的一项研究比较了接受相同监督、门诊肺康复计划的IPF患者与匹配COPD患者的反应。并确定完成肺康复或对肺康复的响应是否与IPF患者的生存期相关。
采用倾向评分匹配法,将纳入肺康复治疗的163例IPF患者与163例COPD对照患者进行1:1匹配。患者接受了为期8周的门诊项目,包括每周两次监督锻炼和教育课程以及额外的无监督家庭锻炼。
基线测量指标(T0)包括BMI,肺活量测定,增量往返步行试验(ISW),慢性呼吸系统问卷(CRQ)和虚弱状态(4m步态速度 < 1.0 m/s)。肺康复治疗完成后(T1)测量ISW、CRQ和总体变化评级问卷(GRCQ)。依从性定义为患者参加监督治疗次数。完成肺康复定义为参加肺康复后评估和至少8次监督治疗。肺康复状态定义如下:响应者:完成肺康复,并达到ISW变化的最小重要差异(≥38米);无响应者:完成肺康复但未达到ISW变化的最小重要差异(< 38米);未完成者:未完成肺康复。
研究人员比较了两组的肺康复完成率和疗效。记录IPF队列在肺康复出院后一年内的生存状态。Cox比例风险回归探索肺康复状况与全因死亡率之间的关系。
结果显示,两组的肺康复完成率相似(IPF:69%;COPD:63%;p=0.24)。肺康复治疗后,两组的ISW和CRQ均显著改善,但无组间差异。与COPD组的91%相比,IPF组有88%在肺康复后感觉“好多了”或“稍微好了一点”(p=0.45)。肺康复未完成(HR=5.62, 95%CI, 2.24-14.08)和无响应(HR=3.91, 95%CI, 1.54-9.93)与IPF一年内全因死亡率增加独立相关。根据肺康复状态分层,未完成者和无响应者在1年内死亡比例高于响应者(分别为40%、24%、10%;p < 0.01)。
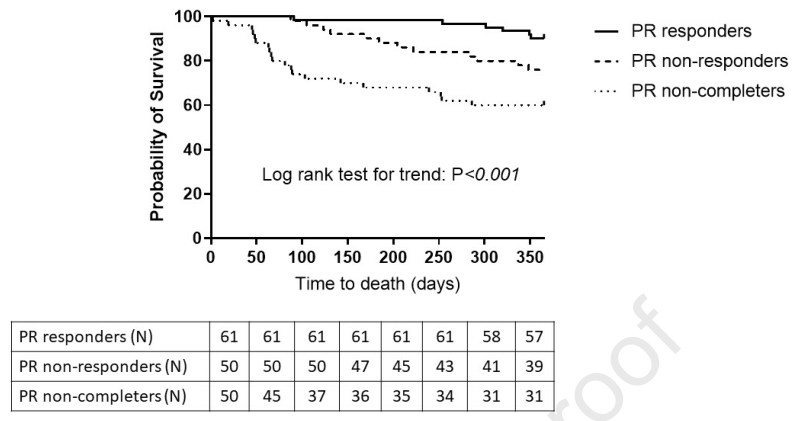
这项真实世界研究数据表明,IPF患者对肺康复的完成率和响应程度与COPD患者组相似。IPF患者肺康复未完成和无响应与全因死亡率增加相关。进一步强化了IPF患者肺康复的益处。
原文出处:
Nolan CM, Polgar O, Schofield SJ, Patel S, Barker RE, Walsh JA, Ingram KA,George PM, Molyneaux PL, Maher TM, Man WDC, Pulmonary rehabilitation in idiopathic pulmonary fibrosis and COPD: a propensity matched real-world study, CHEST (2021), doi: https://doi.org/10.1016/ j.chest.2021.10.021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#特发性#
61
#肺纤维化#
111
#肺康复#
60
#生存期#
61