
在经历了急性脑外伤(TBI)的病人中,长时间的意识丧失是一个不祥的征兆,如果严重的话,可能会导致更坏的结果,包括残疾或死亡。在美国,每年约有900万人因头部创伤到急诊科(EDs)就诊,28.8万人住院,而且这些比率还在增加。TBI的意识障碍( disorder of consciousness,DOC)从昏迷开始,如果持续下去,可能演变成植物人和/或最低意识状态。在较小的环境中,对创伤性脑损伤中持续存在的意识障碍的频率进行了估计,但在更广泛的创伤性脑损伤人群中还没有很好地量化。
在急性住院治疗期间,中度和重度TBI的死亡率为12%至44%。此外,45%至87%的死亡率与撤销维持生命的治疗有关。TBI后急性发生的持续意识障碍与短期和长期的认知和功能缺陷有关。因此,很难确定目前的结果在多大程度上反映了TBI的自然过程,或者说是这些病人的生存和康复状况不佳的自我实现的预言。以前的报告对小样本和TBI后1至10年的长期DOC患者的结果进行了评估。
藉此,美国科罗拉多大学的University of Colorado School of Medicine 等人量化了TBI患者在急诊和重症监护的急性阶段和随后的住院康复期间的意识丧失、与恢复相关的因素和功能能力,包括恢复功能独立性。
他们用DOC评估了31年来在地理上不同的中度或重度TBI患者样本中的中度和重度脑创伤幸存者,这些患者被送入专门医院进行康复治疗。
设计、环境和参与者。这项队列研究分析了加入创伤性脑损伤模型系统国家数据库的创伤性脑损伤患者,这是一个前瞻性的、多年的、纵向的数据库。患者是1989年1月4日至2019年6月19日期间,在参与创伤性脑损伤模型系统项目的23个住院康复中心中的一个,从急性住院出院并进入住院康复的中度或重度创伤性脑损伤幸存者。研究的随访工作一直持续到完成住院康复。
结果。本研究分析的17470名TBI患者,受伤时的中位数(四分位数范围[IQR])为39(25-56)岁,包括12854名男性个体(74%)。
在这些病人中,7547人(57%)经历了最初的意识丧失,其中2058人(12%)持续到康复。那些持续的DOC患者更年轻;有更多的高速损伤(high velocity);有颅内肿块效应、脑室内出血和皮质下挫伤;并且比没有DOC的患者有更长的急性护理。
82%(n = 1674)的昏迷患者在住院康复期间恢复了知觉。
在多变量分析中,与意识恢复相关的因素是没有脑室内出血和颅内质量效应。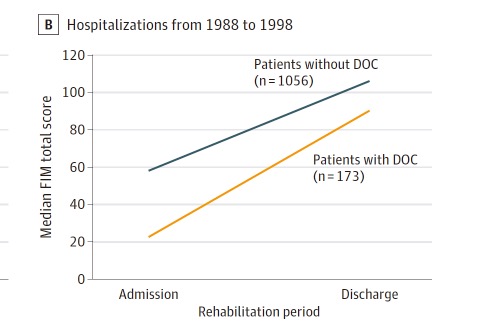
患有DOC的患者的功能改善(从入院到出院的功能独立总分的变化)是+43,而没有DOC的患者是+37(P = .002),2013年患有DOC的患者中有803人(40%)变得部分或完全独立。年轻人、男性、没有脑室内出血、颅内肿块效应和皮质下挫伤与更好的功能结果有关。研究结果在30年的数据库中是一致的。
该研究的重要意义在于,发现了大多数TBI患者最初发生DOC,并在一些患者康复后持续存在,但大多数持续存在DOC的患者在康复期间恢复了意识。这种恢复轨迹可以为急性期和康复期的治疗决策提供参考,并表明在考虑撤回或暂停对TBI和DOC患者的护理时需要谨慎。
原文出处:
Kowalski RG, Hammond FM, Weintraub AH, Nakase-Richardson R, Zafonte RD, Whyte J, Giacino JT. Recovery of Consciousness and Functional Outcome in Moderate and Severe Traumatic Brain Injury. JAMA Neurol. 2021 May 1;78(5):548-557. doi: 10.1001/jamaneurol.2021.0084. PMID: 33646273; PMCID: PMC7922241.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Neurol#
29
#意识丧失#
42
非常受用
61
非常受用
0
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
62
了解一下
58