JAMA Neurology-随访20年发现,小儿多发性硬化症,整体致残率逐渐下降
2021-07-24 Freeman MedSci原创
-随访20年,小儿多发性硬化症,致残率逐渐下降
 小儿多发性硬化症(POMS)的治疗是基于使用在成人中测试过的改变病情的疗法(DMTs)。在许多观察性试验中,这些药物在降低POMS患者的复发率和短期致残率方面显示出很强的效果,其中一些药物对磁共振成像(MRI)病变的积累有保护作用。
小儿多发性硬化症(POMS)的治疗是基于使用在成人中测试过的改变病情的疗法(DMTs)。在许多观察性试验中,这些药物在降低POMS患者的复发率和短期致残率方面显示出很强的效果,其中一些药物对磁共振成像(MRI)病变的积累有保护作用。
只有芬戈里莫德(fingolimod)在随机临床试验(RCT)中进行了测试,显示与干扰素β相比,其在临床和MRI结果上的疗效更高。一些观察表明,当病人接受早期治疗和使用更有效的DMTs时,结果会更好。
在过去的几十年中,新的和日益强大的治疗方法的出现,MS诊断标准的完善,以及治疗模式的改变导致了疾病过程的普遍改善。
到目前为止,在成人多发性硬化症中,随着时间的推移,达到持续残疾的风险逐渐降低;然而,这一发现尚未在POMS人群中得到证实,他们的管理受到18岁以前获批的DMTs数量少的限制,可能还有其他因素,如频繁的认知障碍,家庭参与治疗决策,以及对治疗的低坚持性风险。
藉此 University of Bari Aldo Moro的Damiano Baroncini等人,探究了POMS的病程是否随着治疗和管理标准的变化而发生变化。并评估了POMS患者中,达到持续残疾的时间是如何变化的。
在这个回顾性、多中心、观察性研究中,数据于2019年5月从意大利多发性硬化症登记处提取和收集,这是一个包括59000多名患者的数据库。纳入标准是18岁前发病的MS,2014年1月前诊断,病程至少3年。排除标准是原发性进展型多发性硬化症,发病后一年的扩展残疾状态量表(EDSS)评分至少为8分,无法获得诊断日期,以及少于2次EDSS评分评估。符合条件的患者有4704名POMS患者。根据这些标准,共募集了3198名患者,排除了1506名。
他们按MS诊断的年代(<1993年、1993-1999年、2000-2006年和2007-2013年)比较了达到残疾里程碑(disability milestones )的时间,调整了与EDSS评估和临床疾病活动有关的可能的混杂因素。然后分析了4个诊断年代在人口统计学特征、发病时的临床疾病活动和DMTs管理方面的差异。
共招募了3198名POMS患者(发病时平均年龄为15.2岁;69%为女性;诊断的中位时间为3.2年;前1年和3年的年复发率分别为1.3和0.6),平均(SD)随访21.8(11.7)年。
达到EDSS评分4.0和6.0的中位生存时间为31.7和40.5年。随着时间的推移,达到残疾里程碑的累积风险逐渐下降,无论是EDSS评分4.0和6.0。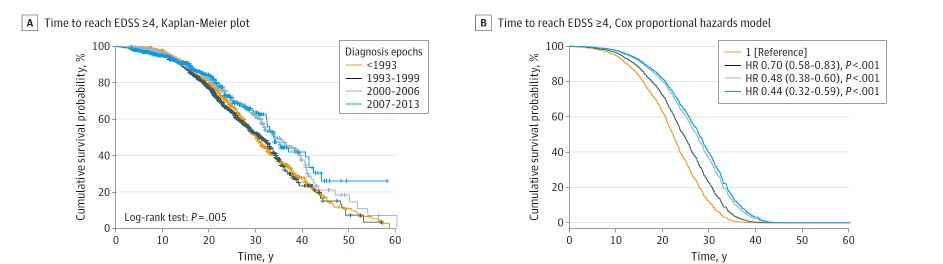
在较晚的诊断年代,有更多的POMS患者接受DMTs治疗,特别是高效力的药物,这些药物的使用时间更早,时间更长。人口统计学特征和发病时的临床疾病活动并没有随着时间的推移而发生明显变化。
这个研究重要意义在于:在POMS患者中,持续残疾的风险在最近的诊断年代减少了50%至70%,这可能是由于治疗和管理标准的改善。
原文出处:
Baroncini D, Simone M, Iaffaldano P, Brescia Morra V, Lanzillo R, Filippi M, Romeo M, Patti F, Chisari CG, Cocco E, Fenu G, Salemi G, Ragonese P, Inglese M, Cellerino M, Margari L, Comi G, Zaffaroni M, Ghezzi A; Italian MS registry. Risk of Persistent Disability in Patients With Pediatric-Onset Multiple Sclerosis. JAMA Neurol. 2021 Jun 1;78(6):726-735. doi: 10.1001/jamaneurol.2021.1008. PMID: 33938921; PMCID: PMC8094039.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
32
#硬化症#
36
#致残#
51
#Neurol#
39
非常受用
66
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
65