SLEEP 2020:失眠患者的福音,Daridorexant的III期临床取得积极进展
2020-08-29 Allan MedSci原创
结果表明,与安慰剂相比,Daridorexant显著改善了睡眠维持时间。
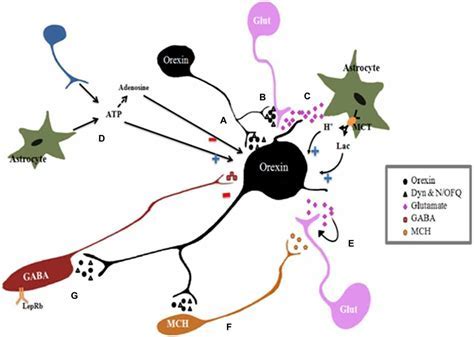
制药公司Idorsia今日宣布,III期临床研究显示,双重Orexin受体拮抗剂daridorexant在成年和老年失眠患者中取得了积极结果。结果将在2020年睡眠会议(SLEEP 2020)上公布。

亨利·福特医院睡眠障碍与研究中心主任Thomas Roth博士评论说:“Daridorexant是一种全新的双重Orexin受体拮抗剂,其药代动力学和药效学特征针对睡眠发作和作用持续时间进行了优化,以提高夜间疗效,而没有残留影响”。
III期临床试验旨在评估daridorexant治疗中度至重度失眠患者的有效性,并评估其安全性。使用多导睡眠监测仪评估睡眠发作后的苏醒(WASO)和持续性睡眠潜伏期(LPS)。睡眠日记问卷用于测量主观总睡眠时间(sTST)。使用最新开发并经过验证的患者报告结局工具“失眠白天症状和影响问卷”(IDSIQ)评估白天功能。结果表明,与安慰剂相比,Daridorexant显著改善了睡眠维持时间。安慰剂、25mg daridorexant和50mg daridorexant患者的WASO(分钟)相对于基线的平均变化分别为-6.2、-18.4和-29.0(在1个月时),在3个月时分别为-11.1、-23.0和-29.4(p<0.0001)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#IDO#
49
#III#
0
#I期临床#
40
#SLE#
43
#II期临床#
47
#III期#
37