Eur Urol:机器人辅助下的根治性肾切除术:比较研究的系统性回顾和元分析
2020-12-04 AlexYang MedSci原创
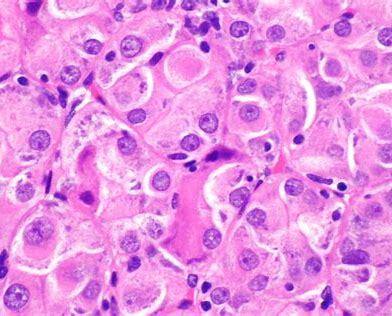
根治性肾切除术(RN)是大面积和局部晚期肾肿瘤的黄金标准治疗方法。尽管机器人辅助下的根治性肾切除术(RRN)应用越来越多,但它是否比标准腹腔镜下根治性肾切除术(LRN)或开放性根治性肾切除术(ORN)
根治性肾切除术(RN)是大面积和局部晚期肾肿瘤的黄金标准治疗方法。尽管机器人辅助下的根治性肾切除术(RRN)应用越来越多,但它是否比标准腹腔镜下根治性肾切除术(LRN)或开放性根治性肾切除术(ORN)更有优势还不清楚。
最近,有研究人员比较了机器人手术与腹腔镜和开放手术在肾细胞癌(RCC)患者中的治疗效果。研究人员在MEDLINE、EMBASE和Web of Science上进行了系统性搜索,寻找了比较RRN与LRN或ORN的回顾性和前瞻性研究。元分析评估了围手术期安全性、有效性、生存率和成本效益结果。分析包括了12个研究,共64221名患者。结果发现,与LRN相比,RRN与显著更长的手术时间(WMD 37.44分钟;p=0.03)、更短的住院时间(WMD -0.84天;p=0.02)和更高的总费用(WMD 4700美元;p<0.001)相关。与ORN相比,RRN与更短的住院时间(WMD -3.06天;p= 0.002)、更少的总体并发症(OR 0.56;p<0.001)、更低的估计失血量(WMD -702 ml;p= 0.01)和更高的医院总费用(WMD 4520美元;p= 0.004)相关。另外,在所有分析中都存在较高的异质性。
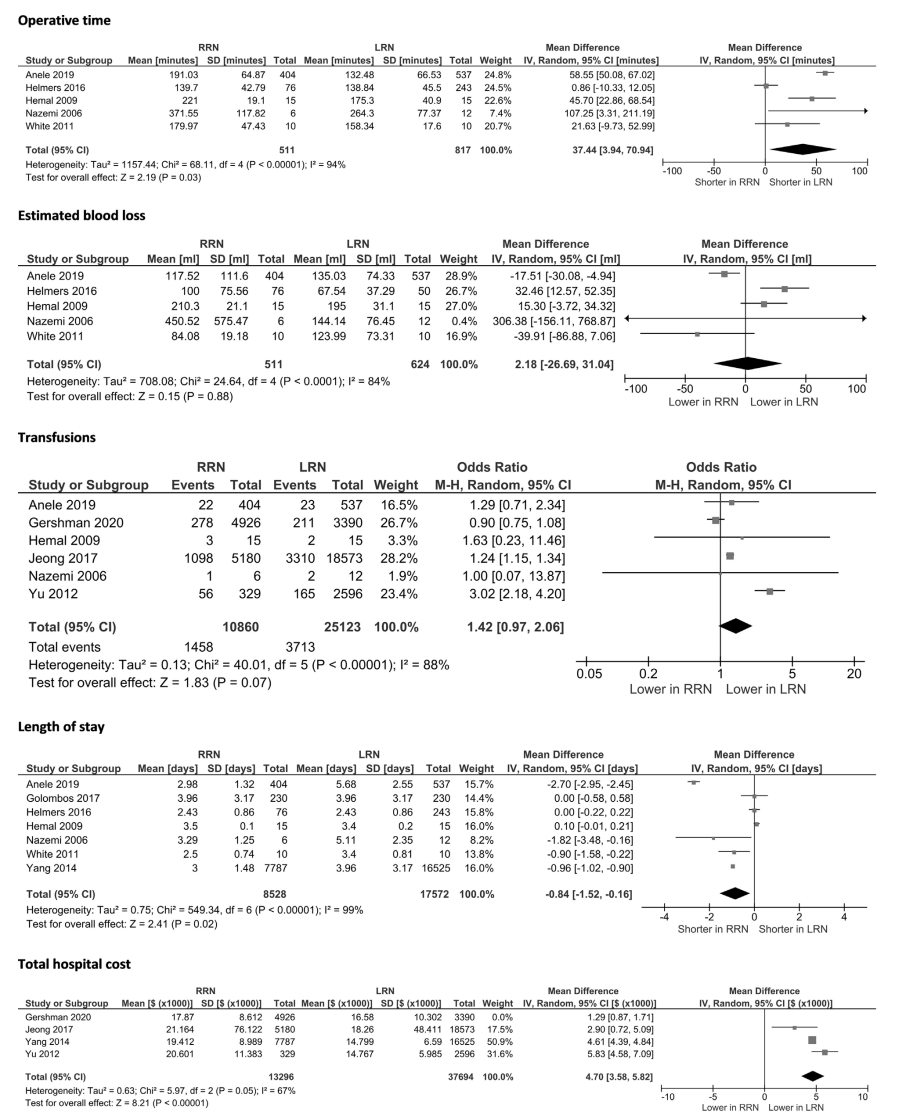
最后,研究人员指出,在接受RN治疗的RCC患者中,与ORN相比,RRN似乎具有一些关键优势,包括更短的住院时间和更少的并发症。与LRN相比,RRN提供了相似的手术结果,但总费用较高。另外,由于研究之间的高异质性和大多数结果的低稳性,这些研究结果应限制在这类分析内进行解释。因此,仍旧需要进行长期跟踪的随机临床研究来获得更确切的结果。
原始出处:
Fabio Crocerossa , Umberto Carbonara , Francesco Cantiello et al. Robot-assisted Radical Nephrectomy: A Systematic Review and Meta-analysis of Comparative Studies. Eur Urol. Nov 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
38
#元分析#
45
#肾切除术#
46
#切除术#
38
#机器人#
26
#机器人辅助#
40
#机器#
32
#根治#
27
受教了~
0