百时美施贵宝公布III期临床研究CheckMate -9LA两年随访数据,结果喜人!
2021-05-20 MedSci MedSci
2021年5月19日,百时美施贵宝公布了III期临床研究CheckMate -9LA两年随访结果。
2021年5月19日,百时美施贵宝公布了III期临床研究CheckMate -9LA两年随访结果。结果显示,与单独接受四周期化疗相比,欧狄沃(纳武利尤单抗)联合伊匹木单抗及两周期化疗能够为一线晚期非小细胞肺癌(NSCLC)患者带来持久的生存获益。在该研究中,接受欧狄沃联合伊匹木单抗及两周期化疗的患者两年生存率达到38%,而接受单独化疗的患者两年生存率为26%。延长随访时间后,接受双免疫联合化疗的患者中位总生存期(mOS,本研究的主要终点)达到15.8个月,而单独化疗组患者的中位OS为11个月(HR:0.72;95% CI:0.61-0.86)。
欧狄沃联合伊匹木单抗及两周期化疗的安全性与免疫治疗及化疗在一线NSCLC的已知安全信息一致。研究结果(摘要#9000)将于美国东部时间2021年6月4日下午1-4点在2021年美国临床肿瘤学会(ASCO)年会上进行口头报告。
CheckMate-9LA研究者、肺部研究德国中心、Grosshansdorf肺科诊所Martin Reck博士表示:“尽管晚期非小细胞肺癌的治疗取得了长足的进步,但仍有很多患者仍无法实现长期生存。基于纳武利尤单抗联合伊匹木单抗在其他III期临床研究中所展现出的持久生存获益,CheckMate -9LA在研究设计的时候将免疫联合治疗与短周期化疗相结合,以期实现对疾病的早期控制。经过两年的随访,我们进一步看到了这种疗法的巨大潜力。与单独化疗相比,纳武利尤单抗联合伊匹木单抗及化疗能够持续改善患者的生存。”
延长随访时间后,在接受欧狄沃联合伊匹木单抗及两周期化疗的所有关键亚组中均展示出了具有临床意义的疗效,包括PD-L1<1%和≥1%的患者、鳞癌或非鳞癌患者、以及出现中枢神经系统转移的患者。此外,欧狄沃联合伊匹木单抗及两周期化疗在次要研究终点上也显示出持续的改善,包括无进展生存期(PFS)和客观缓解率(ORR);在探索性研究终点持续缓解时间(DoR)上同样如此:
- PFS:在随访两年时,与单独化疗相比,患者接受欧狄沃联合伊匹木单抗及两周期化疗后,疾病进展或死亡风险降低33%(HR:0.67; 95% CI:0.56-0.79)。
- ORR:与单独化疗相比,更多患者对欧狄沃联合伊匹木单抗及两周期化疗产生应答(免疫联合化疗为38%,单独化疗为25%)。
- DoR:患者接受欧狄沃联合伊匹木单抗及两周期化疗,DoR延长至13个月,而单独化疗患者的DoR为5.6个月。
延长随访时间后,未观察到新的安全性信号或与治疗相关的死亡病例。在接受欧狄沃联合伊匹木单抗及两周期化疗的患者中,3-4级治疗相关不良事件出现的比例为48%,而在接受单独化疗的患者中,这一比例为38%。
百时美施贵宝副总裁、胸部肿瘤开发负责人Abderrahim Oukessou博士表示:“针对转移性癌症的研究目标是进一步改善患者的生存期,让难于被诊断的疾病,如晚期非小细胞肺癌,实现更长的生存。在今年的ASCO会议上,我们将公布多项III期临床试验的结果。这些结果表明,欧狄沃联合伊匹木单抗能够为多种癌症的患者带来显著且持久的获益。CheckMate -9LA研究的2年随访结果令我们感到非常鼓舞,其数据进一步表明,这项独特的联合疗法可以持续为非小细胞肺癌患者带来显著获益。”
目前,欧狄沃与伊匹木单抗组合疗法已在6项III期临床研究中展示出显著的总生存获益,分别是CheckMate -9LA和CheckMate -227(非小细胞肺癌)、CheckMate -067 (转移性黑色素瘤)、CheckMate -214(晚期肾细胞癌)、CheckMate -743(恶性胸膜间皮瘤)和CheckMate -648(食管鳞状细胞癌)。
备注:伊匹木单抗尚未在中国上市
关于CheckMate -9LA
CheckMate -9LA是一项开放、多中心、随机III期临床研究,该研究在不考虑患者PD-L1表达水平与组织学类型的情况下,评估与单独化疗相比(最多四个周期,适用的患者后续可选培美曲塞进行维持治疗),纳武利尤单抗(360mg,每三周一次)与伊匹木单抗(1 mg/kg,每六周一次)联合化疗(两个周期)一线用于转移性非小细胞肺癌(NSCLC)患者的治疗效果。试验组患者(n=361)接受最多两年的免疫治疗,直到出现疾病进展或不可耐受的毒性。对照组的患者(n=358)接受最多四个周期的化疗并可选择性接受培美曲塞维持治疗(如适用),直到出现疾病进展或不可耐受的毒性。该试验的主要研究终点是意向治疗人群的总生存期(OS)。次要关键研究终点包括无进展生存期(PFS)和客观缓解率(ORR),并且该试验基于生物标志物进行了疗效分析。
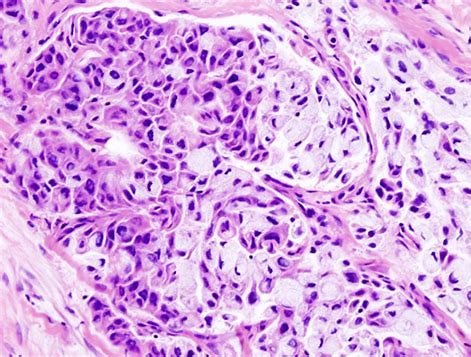
关于肺癌
肺癌是全球癌症死亡的首要原因。肺癌的两种主要类型分别为非小细胞肺癌与小细胞肺癌。非小细胞肺癌(NSCLC)最常见,约占所有肺癌患者的84%。患者的生存率与诊断时的肿瘤分期和组织学类型高度相关。晚期肺癌患者过往五年生存率约为6%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#I期临床#
39
#Checkmate#
39
#III#
30
#III期临床研究#
38
#II期临床研究#
27
#施贵宝#
42
#百时美#
37
#百时美施贵宝#
39
#II期临床#
28
#III期#
27