Clin Gastroenterology H: 储袋炎中粪便钙卫蛋白增加预示着更严重的内镜和组织学疾病进展
2021-12-08 MedSci原创 MedSci原创
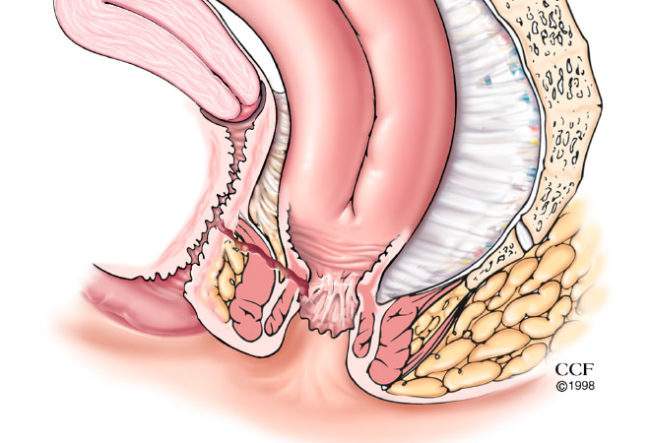
全结直肠切除、回肠储袋肛管吻合术(ilealpouch-analanastomosis,IPAA)是UC病人的首选手术方式。
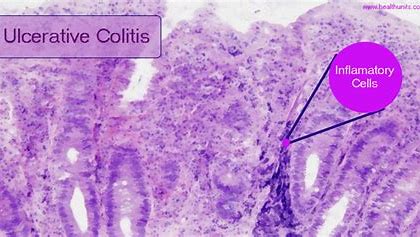
J型回肠-肛门吻合储袋术 (IPAA) 是标准的治疗难治性或复杂性溃疡性结肠炎的手术方式。但是会有多达70%的IPAA患者会发生储袋炎,并且还会出现腹泻、排便次数增多,以及大小便失禁的并发症。目前,对储袋炎症状的评估是通过内窥镜检查进行的,但是其费用非常昂贵而且不便捷。因此,寻找一种准确且具有非侵入性特征的炎症标志物在管理 IPAA的患者中非常重要。在炎症性肠病 (IBD) 患者中,粪便钙卫蛋白 (FC) 越来越多用作内窥镜下评估炎症的替代物,因此,本项研究旨在评估接受 IPAA 的溃疡性结肠炎患者 FC 水平与储袋炎症之间的关联。
研究人员进行了一项针对接受IPAA并完成J 型储袋手术的成人溃疡性结肠炎的临床研究,前瞻性地进行了随访。所有患者在FC采样后90天内进行了临床、内窥镜和组织学评估。储袋炎定义为储袋炎疾病活动评分≥7(最高分:18)。

总体而言,156 名患者有296 份样本符合纳入标准。共有 52% 的患者为男性,评估时的中位年龄为 43(IQR,35-58)岁,中位储袋年龄为 10( [IQR],2.5-15)年。与储袋炎患者相比,未患储袋炎患者的中位 FC 值显着降低(208 [IQR,96-478] μg/g vs 550 [IQR,250-1051] μg/g;P< .0001)。内窥镜和组织学评分较高的患者的FC平均值明显增加。作为储袋炎的预测指标,FC的表现优于C反应蛋白。>460μg/g 的FC具有很高的预测特异性(Pouchitis 疾病活动评分内镜子评分≥5),而且<125μg/g 的FC在预测内镜缓解方面具有超过 80%的特异性。
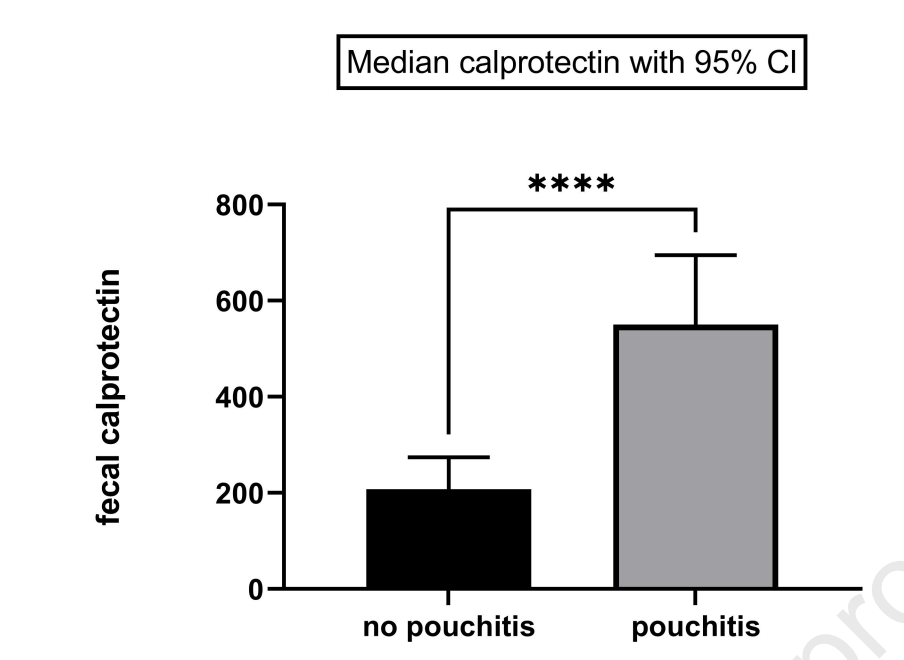
本项研究通过前瞻性的研究证实溃疡性结肠炎患者接受IPAA手术后再内窥镜和组织学中存在处袋炎症的FC水平会升高。FC 可能是管理 IPAA 后患者的有用工具。
原始出处:
Jacob E. Ollech. Et al. Fecal Calprotectin Is Increased in Pouchitis and Progressively Increases With More Severe Endoscopic and Histologic Disease. Clinical Gastroenterology and Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AST#
35
#组织学#
41
#GAS#
34
#疾病进展#
30
#Gastroenterol#
39
受教了
42
#内镜#
34
#粪便#
29
#Gastroenterology#
26