Annals of Neurology:阿尔茨海默病潜在治疗靶点:后内侧、前颞网络
2021-10-26 MedSci原创 MedSci原创
后-内侧和前-颞网络在阿尔茨海默病的病理生理学和临床症状中的关键作用。
海马是一个复杂的结构,连接到两个皮质网络,即前-颞(AT)和后-内侧(PM)网络。内嗅皮质和周围皮质的前-外侧部分主要连接到AT皮质网络,包括前腹外侧颞皮质,外侧眶额皮质和杏仁核。内嗅皮质和海马旁皮质的后内侧部分主要连接到PM皮质网络,包括默认模式网络(DMN)区域,以及丘脑和枕叶皮质。AT网络更多地连接到海马前部,而PM网络更多地连接到海马后部。AT和PM网络在阿尔茨海默病(AD)病理生理学方面特别重要。AT和PM网络之间的相互作用对情景记忆形成至关重要,最近的研究表明,在认知正常的老年受试者中,AT和PM网络选择性地易受AD病理学的影响,tau针对AT网络,然而,淀粉样蛋白-β病理学优先影响PM网络。
Gaël Chételat等在Annals of Neurology杂志发表研究文章,评估了AT、PM这两个网络的功能改变,它们随时间的变化,以及与阿尔茨海默病的认知的联系。
该研究采用静息状态功能性磁共振成像、横断面和纵向研究方法,对53例 β 淀粉样蛋白阳性的老年痴呆患者和68例健康老年人进行MTL连接评价。首先,比较了对照组的后-内侧和前-颞网络的功能连接。其次,比较了这些网络之间的功能连接,以及基线和18个月随访病人之间的功能连接。评估了两个网络之间连接变化的联系,以及认知表现。
该研究发现患者的海马和后-内侧神经网络之间的连接降低,同时几个MTL亚区和前-颞神经网络之间的连接增强。
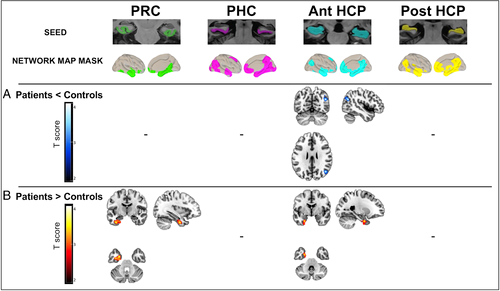
与健康老年对照组相比,阿尔茨海默病患者内侧颞叶(MTL)亚区功能连接的横断面改变。组间差异图显示,与对照组相比,患者的边缘皮质(PRC)、海马旁皮质(PHC)和海马(HCP)的连接性显著降低(蓝色至白色标度)(A)或增加(红色至黄色标度)(B)。
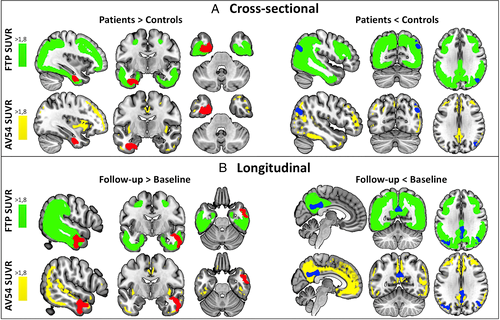
患有轻度认知障碍和AD痴呆的淀粉样蛋白-β阳性患者中氟哌啶醇的最高标准摄取值比值(SUVR)区域(绿色),以及阿尔茨海默病中氟哌啶醇的最高SUVR区域(黄色)。患者功能连接增加的结果(红色,左侧)与tau沉积最高的区域重叠。患者连接降低的结果(蓝色,右侧)与tau沉积最高的区域和淀粉样蛋白沉积最高的区域重叠。患者连接降低的结果(蓝色,右侧)与tau沉积最高的区域和淀粉样蛋白沉积最高的区域重叠,MTL-后-内侧连接减弱和 MTL-前-颞侧增强都预示着认知能力的下降。
MTL-后-内侧连接减弱和 MTL-前-颞侧增强都预示着认知能力的下降。此外,后-内侧和前-颞网络的变化是相互关联的,如MTL-后-内侧连接减弱与MTL-前-颞侧连接增强相关。
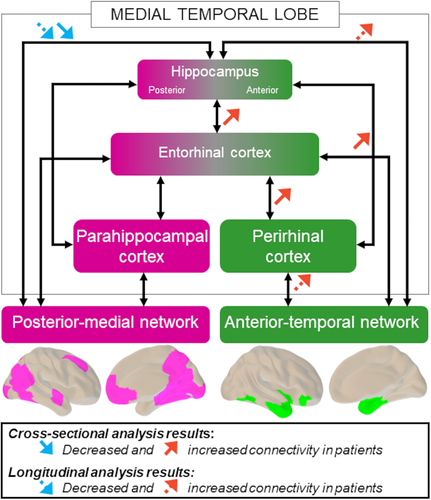
与对照组相比,患者组颞叶内侧亚区连接的横断面改变用实箭头表示。从基线到随访患者的纵向变化用虚线箭头表示。连接减弱(蓝色箭头)主要影响后-内侧网络,而连接增强(红色箭头)主要影响前-颞网络。
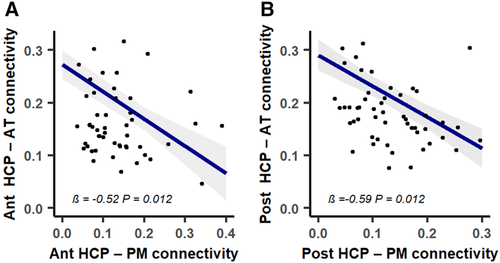
随着时间的推移,患者内侧颞叶(MTL) -后-内侧(PM)连接减弱,而MTL-前-颞叶(AT)连接增强。前、后海马(HCP)-PM网络连接减弱分别预测了前、后HCP-AT网络连接的增强。蓝线代表线性混合效应模型的拟合回归。
Gaël Chételat等通过对阿尔茨海默病淀粉样β-阳性患者的横截面和纵向分析,提供MTL分区功能连接的研究。该研究首次在AD中发现AT、PM与MTL连接随时间的变化(MTL-AT增强和MTL-PM减弱)。MTL-PM连接减弱MTL-AT连接增强是两种相互关联的机制。重要的是,MTL-PM和MTL-AT的变化都与AD相关的认知下降有关。这些结果揭示了后-内侧和前-颞网络在阿尔茨海默病的病理生理学和临床症状中的关键作用。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
36
#阿尔茨#
38
#阿尔茨海#
32
#治疗靶点#
42
#阿尔茨海默#
30
AD的研究任重道远
63