2022年4月24日,中国临床肿瘤学会(CSCO)正式发布了《肿瘤相关性贫血实践指南2022》,本次指南的修订旨在进一步提高肿瘤相关性贫血诊疗规范水平,保障医疗质量安全,为维护患者健康权益提供官方依据;同时对规范我国临床诊疗行为具有重要的意义。
相较于2021年版指南,本次更新主要在造血系统恶性肿瘤、 EPO(人促红素/重组人促红素的简称,下同)使用剂量及剂量调整、静脉铁剂使用三个部分,治疗方式的更新升级有望造福更多肿瘤相关性贫血患者:
首先,在肿瘤相关性贫血治疗原则 - 造血系统恶性肿瘤(3.1.2.1)处,对于骨髓异常增生综合征(MDS)IPSS低危、中危-1和WPSS极低危、低危、中危中血清EPO≤500mU/ml的患者,更改方案为“皮下注射EPO 10000U每周3次,或36000U每周1次 或静脉滴注 40000~60000U每周1次“作为Ⅰ级推荐。
其次,在肿瘤相关性贫血治疗手段 - EPO使用剂量及剂量调整(4.2.2)处,EPO起始剂量Ⅰ级推荐增加“40000U每周一次,皮下注射或静脉滴注”。
第三,在肿瘤相关性贫血治疗手段 - 静脉铁剂使用剂量、途径及注意事项(4.3.3)中,增加异麦芽糖酐铁的用法用量。
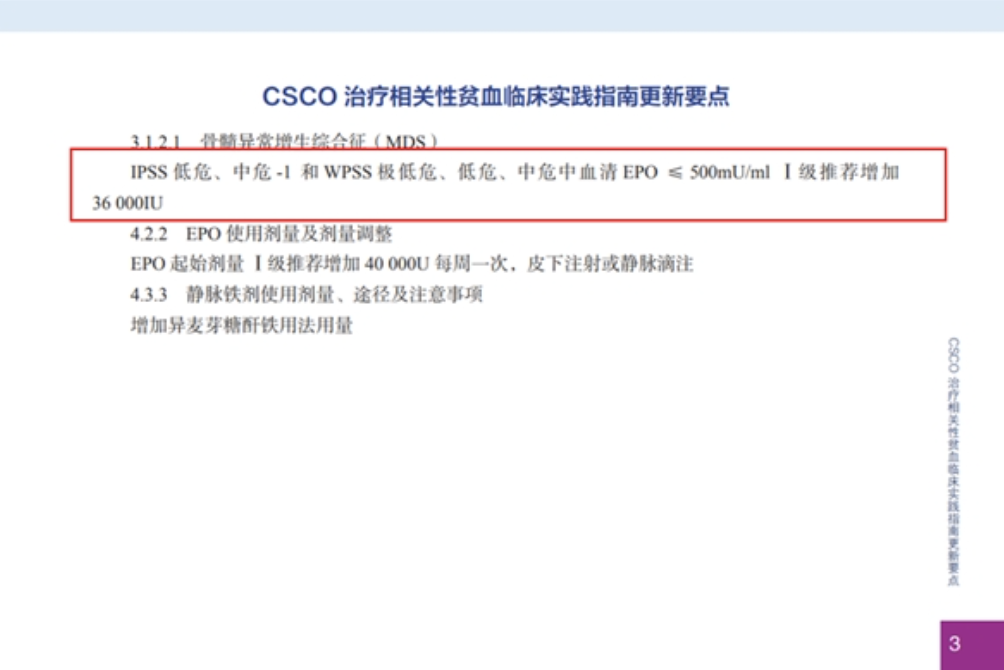
36000 U每周一次成为MDS的 I级推荐新方案
2021版指南中对于MDS仅推荐“皮下注射EPO 40 000~60 000U,每周1-2次”用于治疗低中危MDS贫血。在本次更新中,针对因频繁皮下注射的给药方式,导致患者依从性较差的特点,首次出现了两种不同给药方式的推荐:36 000U每周1次,或静脉滴注 40 000~60 000U每周1次。36 000 U规格因其便利性及经济性受到了医疗工作者的认可;静脉滴注在减轻患者注射痛苦的同时,也在一定程度上减轻医务人员的工作量,节约医疗资源。
首都医科大学附属北京红十字朝阳医院陈文明教授表示:“EPO一直是MDS贫血有效的治疗药物,但由于是注射剂型,再加上几乎每天都需要使用,导致部分患者依从性较差,在一定程度上影响治疗效果和预后, 36000U剂型能很好解决这个问题,希望36000U的EPO能造福更多的MDS贫血患者。”
浙江省中医院周郁鸿教授表示: “EPO是临床上治疗多种疾病引起的贫血,尤其是治疗低/中危骨髓异常综合征致贫血患者的主要药物之一,以往EPO以短效为主,剂量偏小,需每天或隔日皮下注射,患者依从性较差,在一定程度上也影响了治疗效果和预后。EPO 36000单位/针, 每周1—2次皮下注射,减少注射次数,提高患者依从性,既便利又经济。目前36000U入选了CSCO肿瘤相关性贫血临床实践指南,给我们医护人员提供又一优质的武器,给病人带来福音。我深信必将受到全国临床专家和贫血患者的高度关注。“
EPO起始使用剂量上调,新增“静滴“用药方式
在上一版指南中,EPO推荐方案均为皮下注射方式,10000 U每周三次的频率使得患者依从性较差,且国内医疗机构对床位周转率有一定要求、导致患者无法接受足量足疗程的治疗,从而使CRA治疗效果不理想。本次《肿瘤相关性贫血实践指南2022》EPO 起始剂量新增“40 000 U每周一次,皮下注射或静脉滴注”
中国科学院大学附属肿瘤医院(浙江省肿瘤医院)肿瘤内科主任医师张沂平教授表示:“当Hb≤100g/L即可启动EPO治疗,常规治疗方案可选择EPO 36000U或40000U作为起始剂量,1个疗程4-6周。本次指南新增的每周一次EPO 40000U静脉滴注用法用量,更加符合目前的医疗环境,尤其是现在疫情反复的情况下,能够降低患者访视成本和疫情风险,提高患者的依从性,节约医疗资源,提高床位周转率,值得临床推广。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
32
#实践指南#
38
请问从哪里找这本指南呢
64
#临床实践#
43
#临床实践指南#
47