JCC:乌司奴单抗(Ustekinumab)在溃疡性结肠炎中的有效性和安全性分析
2021-04-18 MedSci原创 MedSci原创
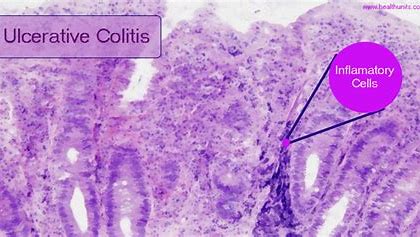
炎症性肠病(IBD)包括克罗恩病(CD)和溃疡性结肠炎(UC),是一种主要累及胃肠道系统的慢性进展性疾病,可引起包括狭窄、脓肿、瘘管等并发症。
炎症性肠病(IBD)包括克罗恩病(CD)和溃疡性结肠炎(UC),是一种主要累及胃肠道系统的慢性进展性疾病,可引起包括狭窄、脓肿、瘘管等并发症,并增加患者罹患肠道肿瘤风险,近半数患者在前10年内需要手术而且术后复发的风险达50%,近年流行病学数据发现发病率逐年上升,且主要受累人群为青壮年,疾病的治疗为患者和社会均带来严重负担。
传统治疗药物虽能改善症状,但不能阻止潜在的炎症进程,生物制剂(TNF抑制剂)的出现极大改变了IBD的治疗方式和治疗目标,可诱导患者临床缓解,达到肠道黏膜愈合,减少手术率与住院率。2019年英夫利西单抗进入国家医保范围,增加了生物制剂对于IBD患者的可及性,但仍有一定比例患者因为药物机制或免疫介导药物代谢动力学原因导致继发性失应答,仅依靠抗TNF单抗仍无法完全满足临床上医生和患者对改变IBD疾病进程的需求。
乌司奴单抗(Ustekinumab)是全球首个全人源“双靶向”IL-12和IL-23抑制剂,早在2008年获得美国食品药品监督管理局(FDA)批准用于治疗银屑病,2016年被批准用于治疗活动性CD,2020年3月在中国获批CD适应证。全球性III期临床研究(UNITI-1、UNITI-2和IM-UNITI)显示,乌司奴单抗治疗CD能够快速改善症状并持续维持缓解,降低患者住院率和手术率,改变疾病进程。因此,本项研究旨在探究在现实生活中乌司奴单抗(ustekinumab)在UC中的有效性和安全性。
研究人员将ENEIDA登记册中的患者前瞻性的纳入本项研究,这些患者均处于活动期UC [Mayo评分> 2]并接受了至少一次静脉注射剂量的ustekinumab治疗。临床活动和有效性是基于Mayo评分进行测量的,并在接受治疗的第16周评估了药物反应。
本项研究共包括95名患者。在第16周,有53%的患者有临床缓解反应。在多变量分析中,血清C反应蛋白升高是唯一显着降低缓解率的危险因素。在第24周和第52周,分别有39%和33%的患者实现了疾病缓解。在随访时间内,有36%的患者中止了ustekinumab的治疗。87%的患者在第16周维持了ustekinumab治疗,而在第56周时只有63%的患者继续接受治疗,在第72周时为59%,患者临床疾病不能获得缓解是ustekinumab停用的主要原因。
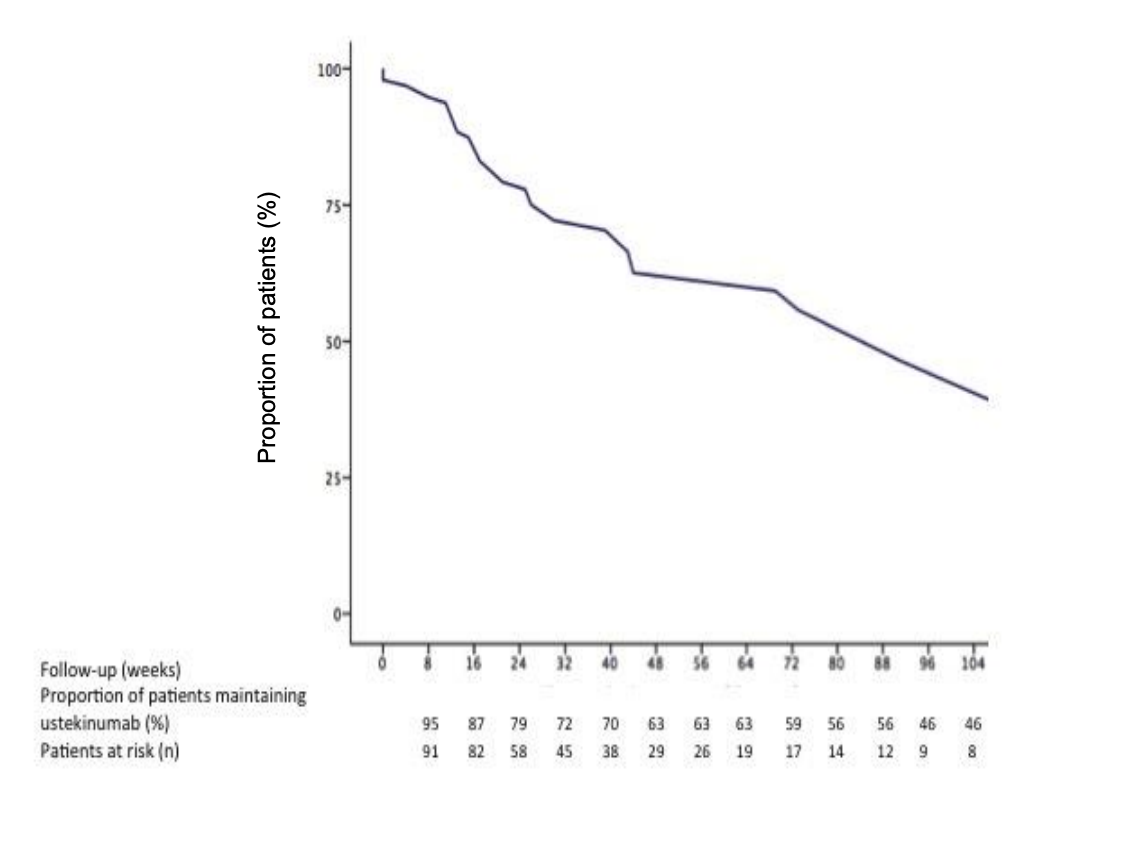
图:乌司奴单抗治疗溃疡性结肠炎随着时间的疗效变化
本项研究证实Ustekinumab在现实生活中无论短期还是长期都有很好的缓解疾病活动的效果,但是基线时较高的炎症负担与获得缓解的可能性较低相关。
原始出处:
María Chaparro. Et al. Effectiveness and safety of ustekinumab in ulcerative colitis: Real-world evidence from the ENEIDA registry. Journal of Crohn's and Colitis.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










几个权威指南没有明确推荐乌司奴在UC中应用呀
40
#溃疡性#
29
#mAb#
27
#ustekinumab#
40
好的
57
太棒了
64