小儿间断性呼吸困难还可能是因为……
2017-12-01 熊长明 肺血管病
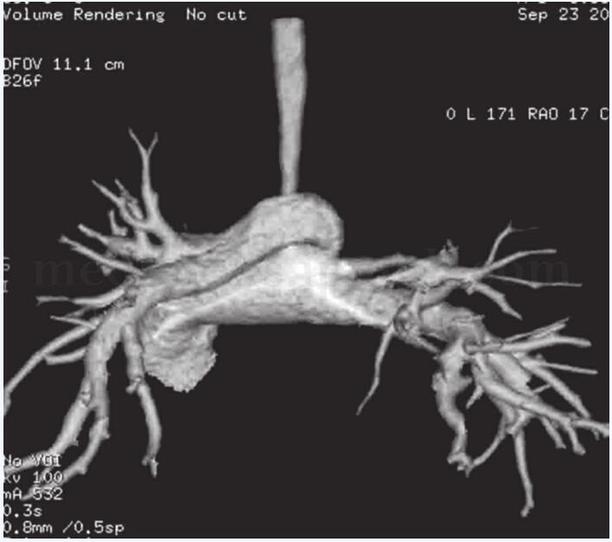
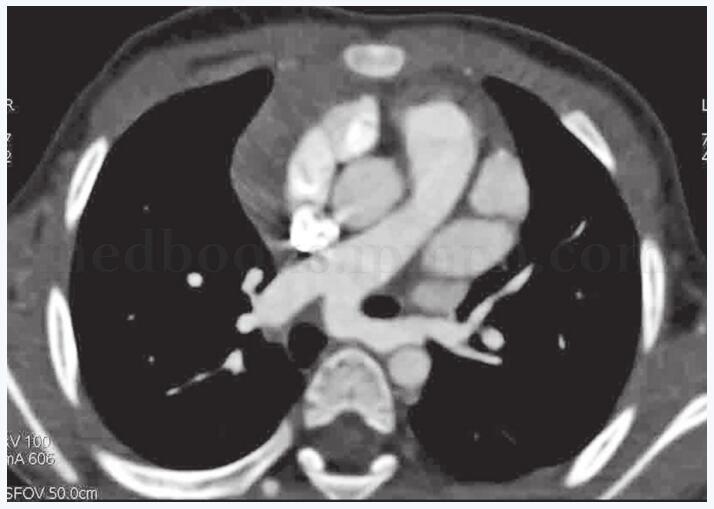
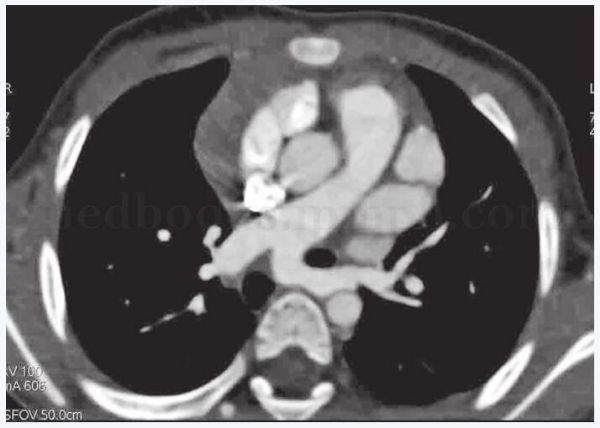
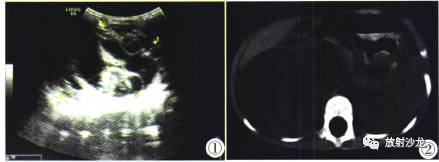
患儿,女,1岁。因生后间断性呼吸困难,怀疑先天性心脏病就诊。经诊断心内结构未见明确异常,而是由一种罕见的先天性肺血管畸形所造成。详见以下病例——

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#间断#
25
#间断性#
40
#呼吸困难#
42
非常好的文章.学习了
78