Nature:科学家首次证实正常的LRRK2基因也会促进帕金森病,90%发病原因不明的患者或许也有救了
2018-08-07 奇点糕 奇点网
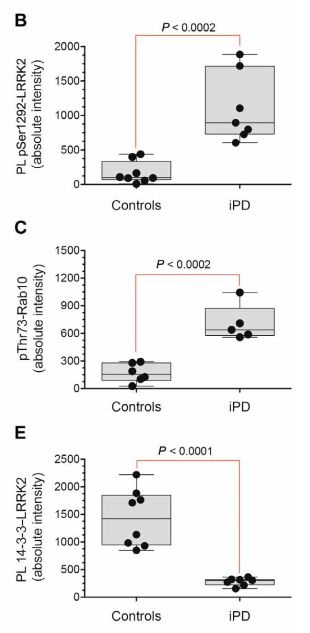
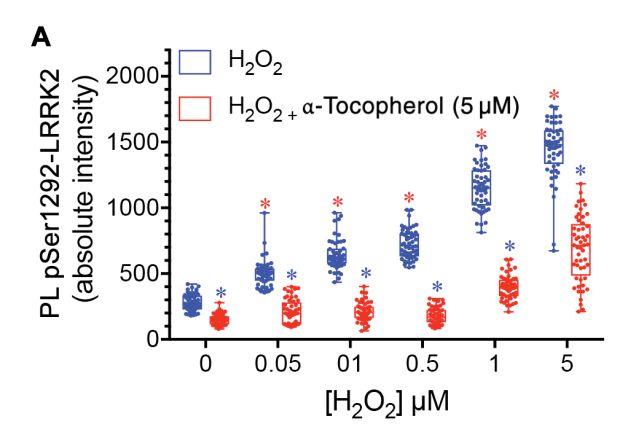
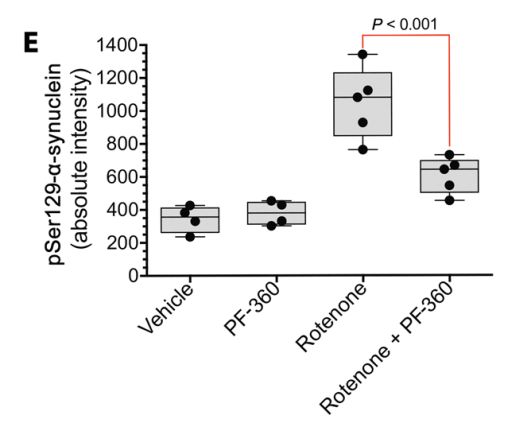
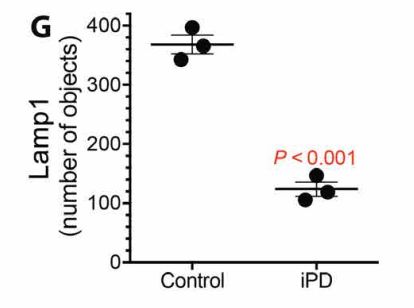
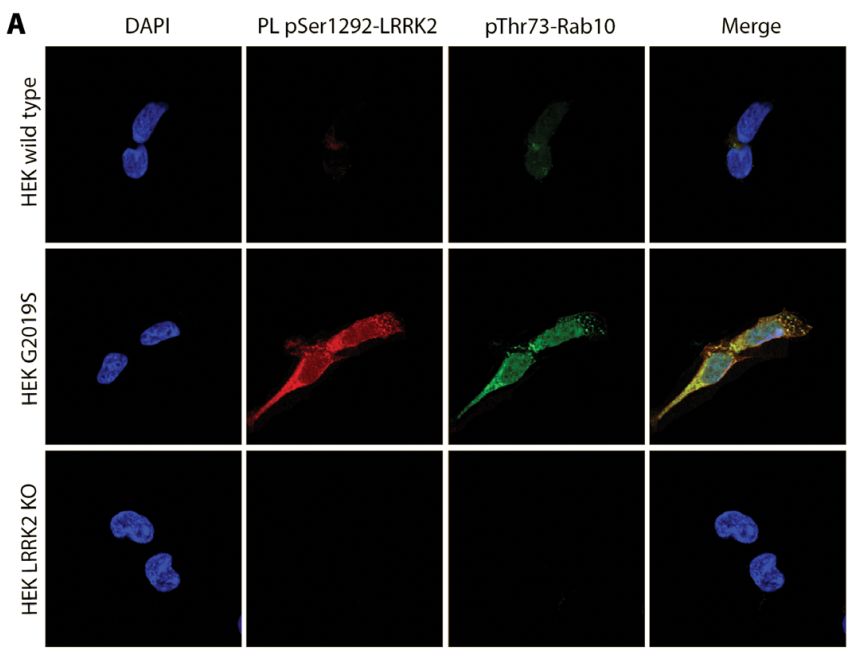
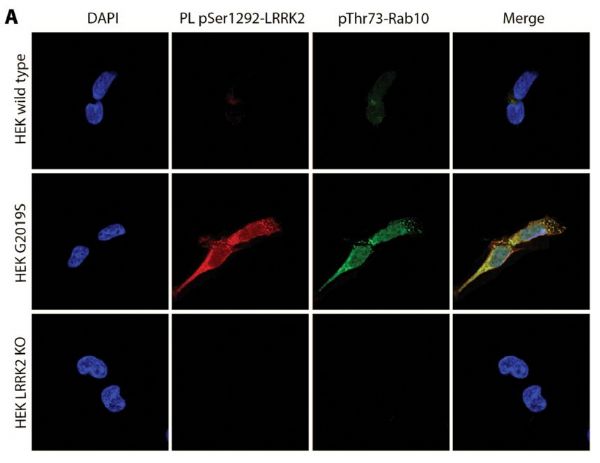
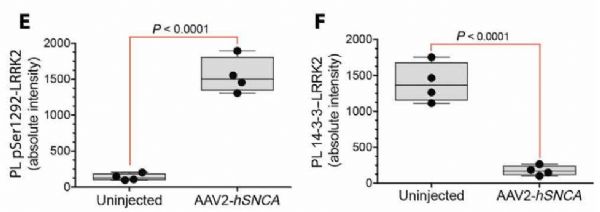
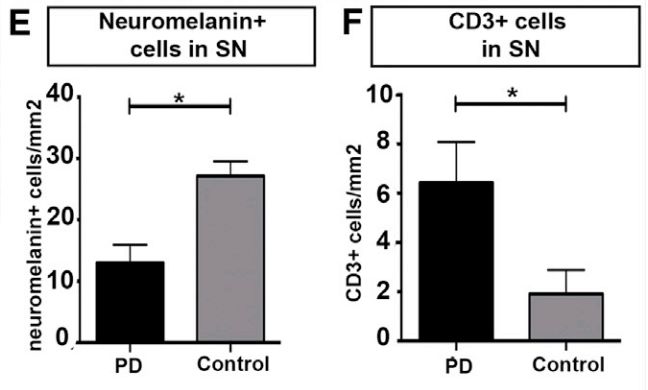
近期的《科学转化医学》刊登了匹兹堡大学研究者的新发现——无论是否突变,LRRK2都在帕金森病发展中有关键作用,无突变的特发性帕金森患者也存在LRRK2蛋白过度激活,神经元细胞自噬功能受损,导致α-突触核蛋白的异常积累,参与帕金森疾病发展!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#首次证实#
39
#Nat#
27
学习了谢谢
85
向科研者致敬!!!
89
学习了!!!
94
知之为知之
77