2019年ESMO-GI:TAS-118联合奥沙利铂显著延长晚期胃癌患者的生存期
2019-07-11 Allan MedSci原创
根据2019年欧洲肿瘤内科学会胃肠癌大会(ESMO-GI)上发表的一项研究,TAS-118联合奥沙利铂作为晚期胃癌患者的一线化疗方案,显著提高了患者的生存率。
根据2019年欧洲肿瘤内科学会胃肠癌大会(ESMO-GI)上发表的一项研究,TAS-118联合奥沙利铂作为晚期胃癌患者的一线化疗方案,显著提高了患者的生存率。TAS-118是一种含有S-1的口服药物,S-1是一种氟嘧啶制剂,含有替加氟、5-氟尿嘧啶、吉美嘧啶、奥替卡西的前药以及甲酰四氢叶酸。
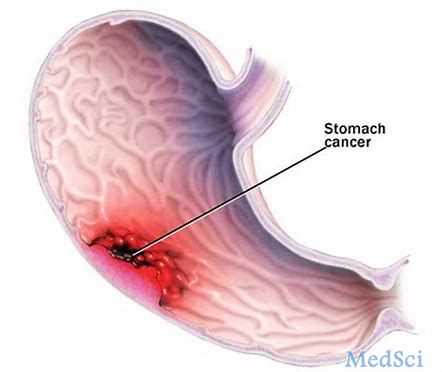
胃癌早期症状包括胃灼热、上腹疼痛、恶心及食欲不振。症状与消化性溃疡类似,是导致延误就医与高死亡率的原因。但其痛感与溃疡有差异,胃溃疡是食后痛而十二指肠溃疡是空腹痛,但胃癌通常不受进食的明显规律影响,且其痛感是一种咬合性疼痛并且制酸剂不能解除痛感,然而还是有较少数胃癌痛感会受进食有些许影响并且制酸剂能稍微缓解。所以胃镜是唯一有效的诊断方法。
原始出处:
http://www.firstwordpharma.com/node/1652387#axzz5tMRLVCBr
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#铂#
38
#SMO#
30
#胃癌患者#
31
#晚期胃癌#
37
#ESMO#
25
#生存期#
31
#S-1#
25
#TAS-118#
0